Genomics/Epigenomics
Genomics/Epigenomics
171 - Parent Psychosocial Experiences with Rapid Genome Sequencing
Publication Number: 171.218

Anamika Shah, BA (she/her/hers)
MS-2
Ohio State University College of Medicine
Columbus, Ohio, United States
Presenting Author(s)
Background: Rapid genome sequencing (rGS) in neonatal and pediatric critical care settings is an effective and useful first-tier diagnostic test. In RCTs of rGS, parents report low regret, positive overall experience, reduced uncertainty, and improved empowerment.
Objective: How rGS affects parental psychosocial outcomes when patients are selected at the discretion of the treatment team rather than by the criteria of RCTs is unknown.
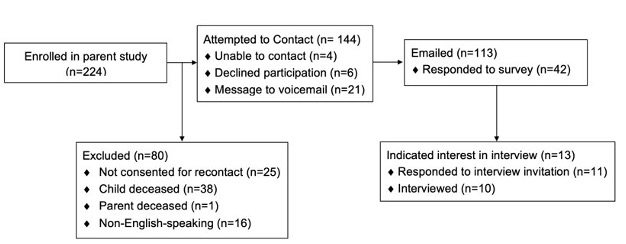
Design/Methods: Parents (N=113) of children (N=71) in neonatal and pediatric intensive care units (median age at consent 0.21 years) who received rGS as part of an existing prospective, non-randomized, validation study (Figure 1) were sent an online survey of previously validated scales (Decision Regret Scale (DRS), Psychological Empowerment Scale (PES), Postpartum Bonding Questionnaire (PBQ)) to measure psychosocial outcomes. Semi-structured interviews were recorded for inductive thematic analysis.
Results:
Response rate was 37% (42/113). Ten respondents completed semi-structured interviews. Fathers made up 33% of survey respondents and 30% of interviewees.
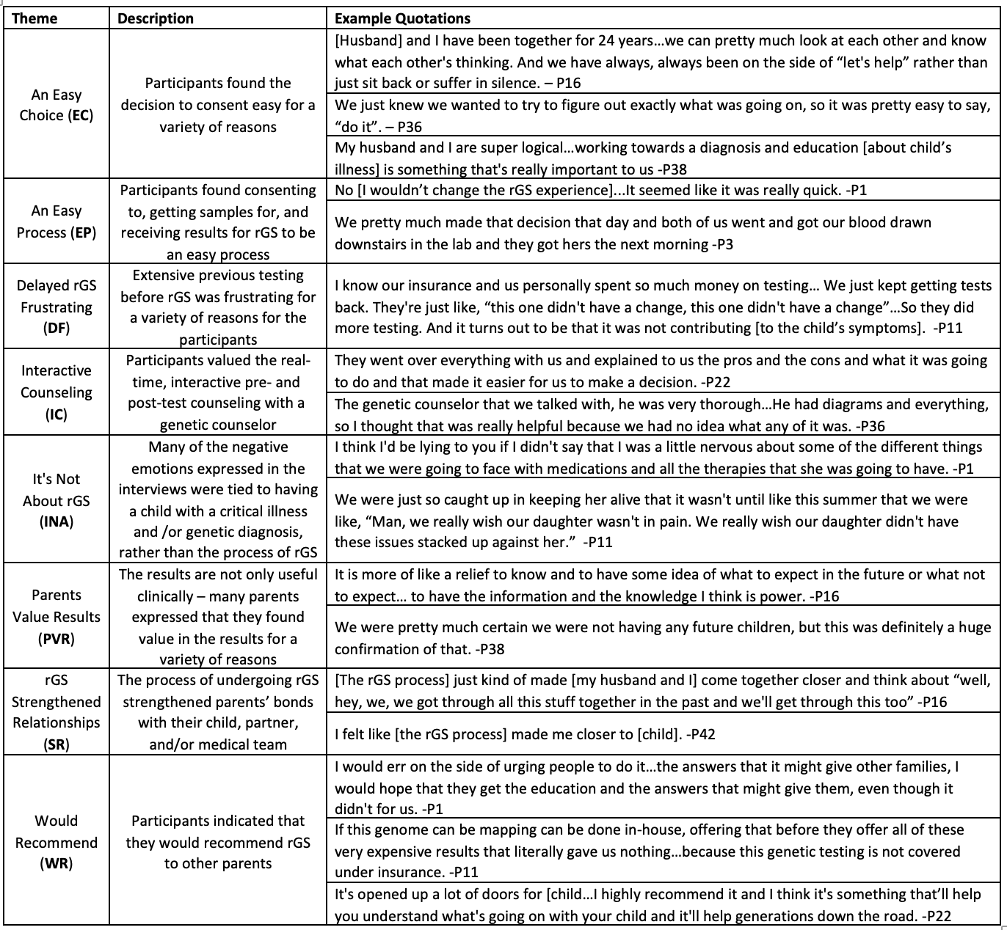
Decisional regret was mild (median DRS=2.08, IQR=0-16.7); half had no regret. Postpartum bonding (median PBQ=1.33, IQR=0.417-2.25) and parental empowerment (median PES=6.25, IQR=5.58-6.92) were high. Outcomes were not correlated with demographics, clinical utility of results, or diagnostic status (Figure 2). Eight themes were identified (Table 1). All parents reported deriving value from rGS results, regardless of diagnostic status. The theme of interactive counseling accounted for 34% of coded quotations.
Conclusion(s):
Parents experience largely positive psychosocial outcomes when rGS is integrated into routine care. rGS does not cause significant psychosocial harm to parents even when there are no actionable results. Outcomes did not differ by gender. Previous studies of parents have focused on mothers and been unable to assess differences by gender.
Several themes arising in the interviews support the value of prioritizing the patient-provider relationship via longitudinal, time-intensive genetic counseling rather than relying on intermittent care conferences or relying solely on neonatologists (Table 1; Themes EC, EP, IC, PVR, SR). Respondents derived value from a variety of rGS outcomes (Table 1; Theme PVR), improving parents’ emotional well-being independent of direct patient benefits.
In summary, we conclude rGS is not harmful to, but rather, beneficial for parent psychosocial well-being in the setting of comprehensive, longitudinal, and interactive pre- and post-test genetic counseling.