General Pediatrics: All Areas
General Pediatrics 1
111 - Prevalence of Using Antibiotics Without a Prescription in a Pediatric Population
Publication Number: 111.114
Stephanie A. Marton, MD, MPH (she/her/hers)
Pediatrician
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background:
Non-prescription antibiotic use (taking antibiotics without a prescription) among pediatric populations is understudied in the United States (US). A previous national, internet-based 2018 survey found that 92% of parents had leftover prescription pediatric antibiotics, and nearly 75% reported giving their leftover antibiotics to other children or adults.
Objective: We studied the prevalence of pediatric non-prescription use in a racially and ethnically diverse sample of parents and caregivers of children under 18 years in safety net clinics in Houston, TX. We explored the sources whereby parents and caregivers obtained antibiotics without a prescription and investigated the symptoms that drive non-prescription use in children. We also explored the types of antibiotics used, the duration of use, and the storage of antibiotics.
Design/Methods: Interviewer-administered surveys were conducted in English and Spanish with parents and caregivers of eligible children receiving care at two Texas Children’s Health Plan clinics in Houston, TX. Interviews occurred from January 2021 to April 2022. Descriptive analysis was used to determine the prevalence of prior pediatric antibiotic non-prescription use, storage practices, and intended reason for antibiotic use (defined as intention to use antibiotics without a prescription or medical guidance for their child).
Results: Of 322 participants surveyed, the majority were female (94%), and the median age was 34 (range 18-69). Participants identified as Hispanic/Latino (51%) and Black/African American (44%) (Table 1). Although few participants (n=3) reported previously using non-prescription antibiotics for their children, 21% reported storing antibiotics at home. Commonly stored antibiotics were: amoxicillin (n=52), clindamycin (n=10), cephalexin (n=4), penicillin (n=3) and trimethoprim/sulfamethoxazole (n=2). 46 (14%) of surveyed participants reported intention to give non-prescription antibiotics to their children. When asked whether a given reason would induce them to give antibiotics to their child without a prescription, the most common reasons were ear infection, bronchitis, and sinus infection followed by fever, urinary tract infection, and sore throat (Figure 1).
Conclusion(s): More than 1 in 5 participants reported storing antibiotics at home, potentially increasing the likelihood of giving antibiotics to a child without consulting a healthcare provider. Our findings reveal some reasons that may drive pediatric non-prescription antibiotic use and will help guide a future antibiotic stewardship intervention to decrease this practice.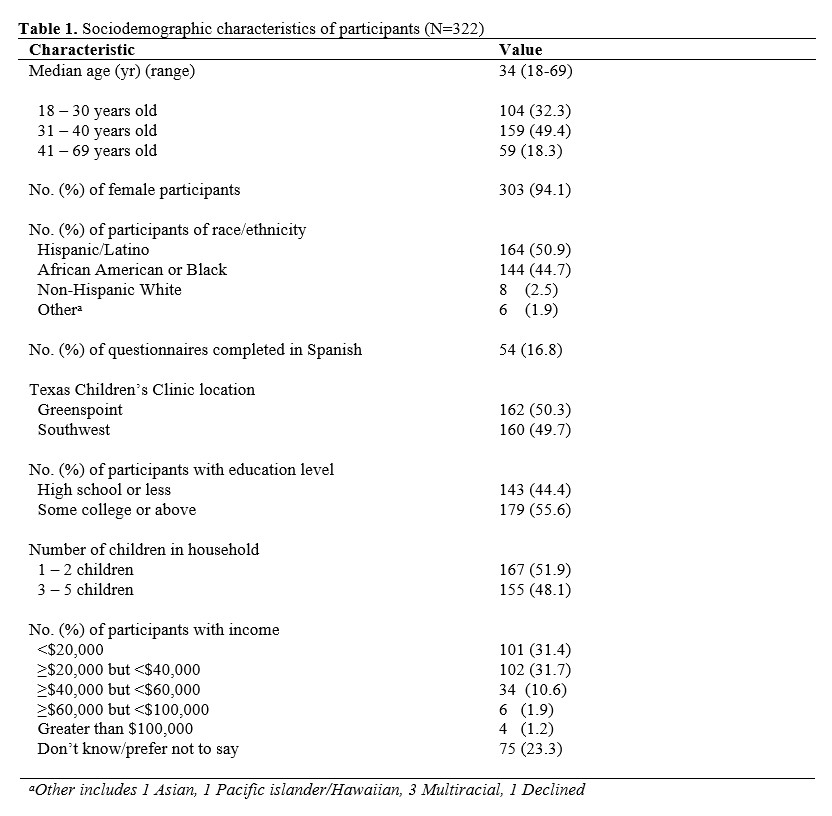
.jpg)
