Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 1: GI Health and NEC Complications
331 - The impact of fetal Inflammatory response on the severity of necrotizing enterocolitis in preterm infants
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 331
Publication Number: 331.133
Publication Number: 331.133
Imran N. Mir, University of Texas Southwestern Medical School, Plano, TX, United States; Mariela sanchez-Rosado, Joe DiMaggio Children's Hospital at Memorial Regional Hospital, Hollywood, FL, United States; Jordan D. Reis, Mednax, Baylor Scott & White Dallas, Dallas, TX, United States; Larry S. Brown, Parkland Health, Dallas, TX, United States; Kate Louise Mangona, University of Texas Southwestern Medical School, Dallas, TX, United States; David B.. Nelson, UT Southwestern Medical Center, Dallas, TX, United States; Myra H. Wyckoff, University of Texas Southwestern Medical School, Dallas, TX, United States; Patti J. Burchfield, University of Texas Southwestern Medical School, Dallas, TX, United States; Sujir Pritha Nayak, UTSW -Dallas, Dallas, TX, United States; Luc P. Brion, UT Southwestern Medical Center, Dallas, TX, United States; Pollieanna M. Sepulveda, University of Texas Southwestern Medical School, Dallas, TX, United States
- IM
Imran N. Mir, MD (he/him/his)
Associate Professor
University of Texas Southwestern Medical School
Plano, Texas, United States
Presenting Author(s)
Background: Neutrophilic infiltration of fetal vessels within the chorionic plate of placenta and umbilical cord vessels, i.e., fetal inflammatory response (FIR), is a pathologic evidence of systemic FIR syndrome. Neonates born with FIR are at increased risk of early-onset sepsis, periventricular leukomalacia and death.
Objective: To determine whether FIR and its severity is associated with severity of necrotizing enterocolitis (NEC) in preterm infants.
Design/Methods: This is a retrospective cohort study of all infants < 33 weeks gestational age (GA) or < 1500 grams birthweight born at Parkland hospital between 2009-2021 who had either suspected or proven NEC. Infants were divided into 3 groups according to modified Bell staging system for classification of NEC (i.e., 1, 2 and 3). Placental pathology was evaluated and gross and histopathologic diagnoses determined. FIR and its severity was diagnosed according to the Amsterdam Placental Workshop Group Consensus Statement: i.e., involvement of chorionic plate vessels, and/or umbilical vein (stage 1); one or both umbilical arteries (stage 2); and presence of fetal neutrophils and/or cellular debris in a concentric ring around at least one of the umbilical vessels (necrotizing funisitis or stage 3).
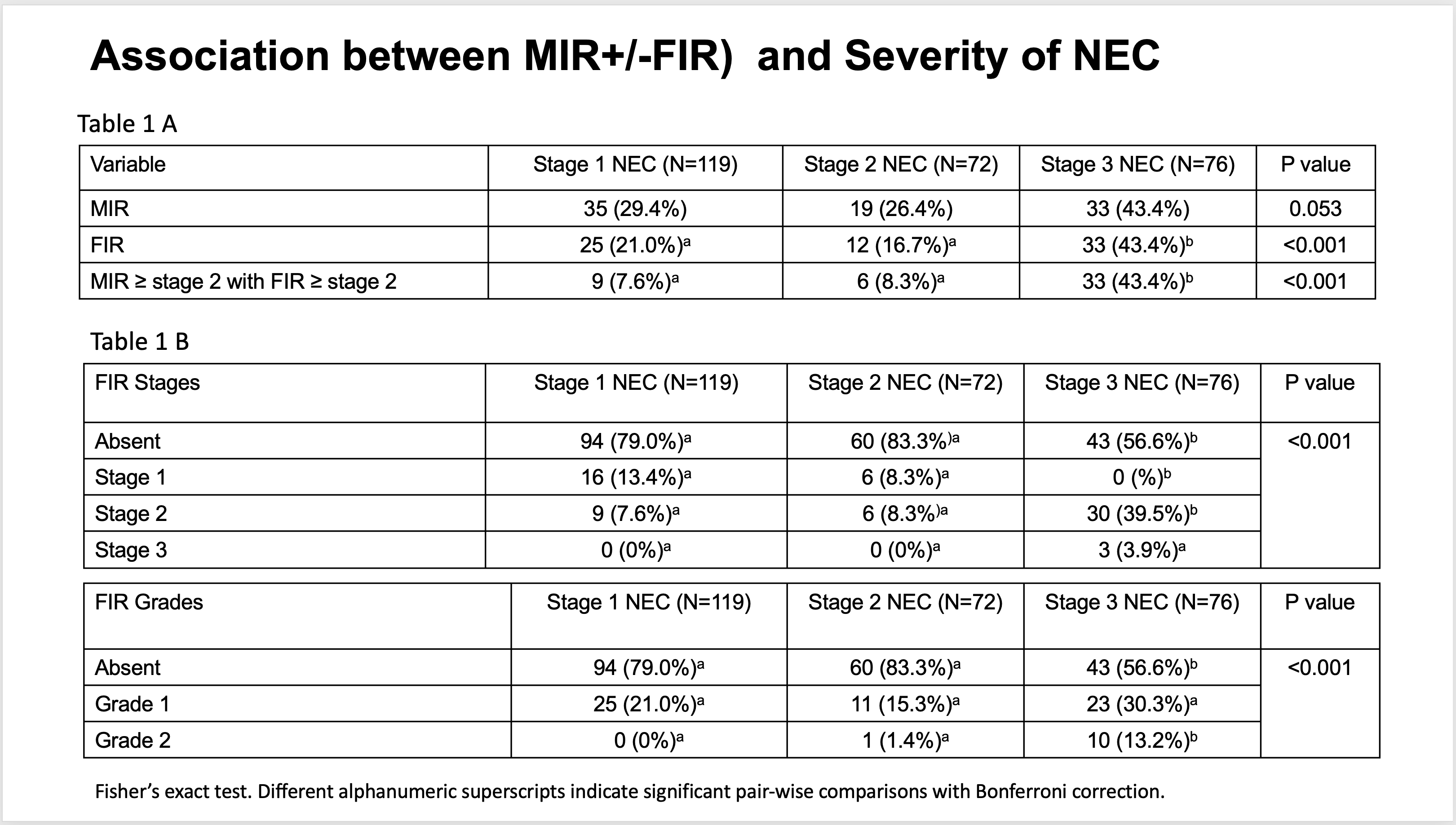
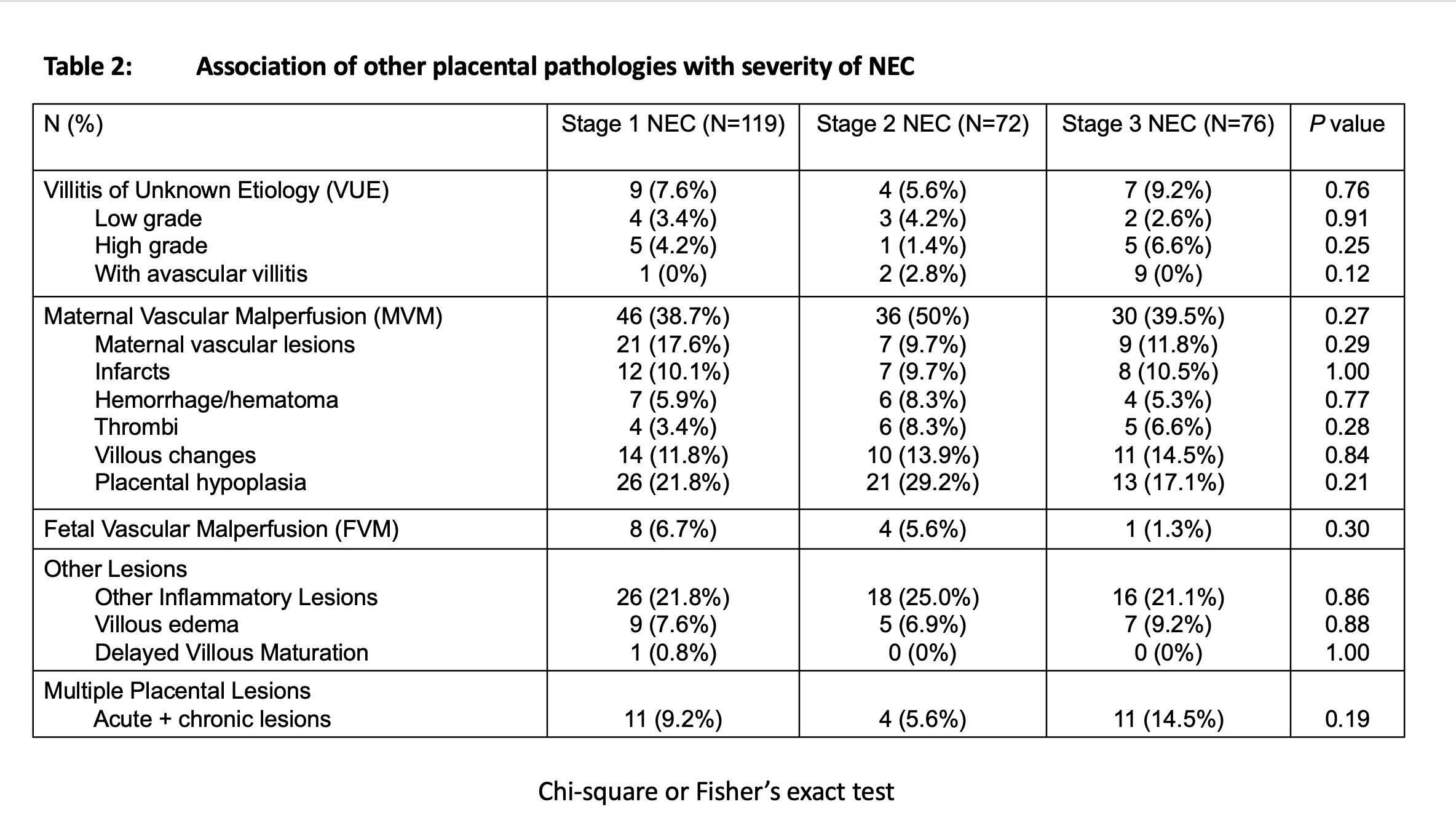
Results: In our cohort (n=267), 119 (44%) infants were diagnosed with stage 1, 71 (27%) with stage 2 and 77 (29%) with stage 3 NEC. Baseline characteristics were similar in infants in all 3 groups except for chronic maternal hypertension (P=0.04), antenatal steroid exposure (P=0.03) and GA (P=0.007). FIR was present in 70 (26.2%) while moderate to severe FIR (i.e., ≥ stage 2 FIR) was present in 48 (18%) infants. Presence of FIR was associated with stage 3 NEC (P< 0.05), and both stage and grade of FIR were associated with stage of NEC (P< 0.0001) (Table 1). On generalized linear model regression, NEC stage was associated with stage of FIR (P< 0.001), but not with GA or z-score of birthweight for GA and sex. Other placental pathologic lesions, including acute histologic chorioamnionitis without FIR or maternal Inflammatory response (MIR), villitis of unknown etiology, maternal vascular malperfusion, fetal vascular malperfusion or other lesions (i.e., villous edema, other inflammatory lesions or delayed villous maturation) were not associated with severity of NEC (Table 2)
Conclusion(s): This is the first report demonstrating the association between increasing severity of FIR and stage of NEC. The possible mechanism for this association could involve gut barrier function, inflammation, and immune dysfunction.