Neonatal Fetal Nutrition & Metabolism
Neonatal Fetal Nutrition & Metabolism 2: Neonatal Nutrition, Growth, and Outcomes
318 - Steroid Exposure in the NICU is Associated with Decreased Fat-Free Mass in Preterm Infants at Discharge
Publication Number: 318.129

Megan Kraemer, DO (she/her/hers)
Neonatal Perinatal Medicine Fellow Physician
Rush Medical College of Rush University Medical Center
Addison, Illinois, United States
Presenting Author(s)
Background:
Systemic corticosteroids are used to facilitate weaning respiratory support in the context of bronchopulmonary dysplasia (BPD) and the treatment of adrenal insufficiency in very preterm infants, despite known side effects. While it is known that corticosteroids increase fat mass in adults, their effect on body composition in very preterm infants has not been well-characterized.
Objective: To compare body composition, measured as fat free mass percentage (%FFM), at NICU discharge in very preterm (VP) infants exposed and not exposed to systemic corticosteroids during hospitalization.
Design/Methods: Prospective study of VP infants born at < 32 weeks gestational age (GA) or with a birth weight (BW) < 1500 grams and admitted to our NICU within 48 hours of life. Exclusion criteria: congenital gastrointestinal anomaly, intestinal perforation, necrotizing enterocolitis, congenital heart disease, and chromosomal abnormalities. We abstracted data from the medical record for anthropometrics, medications, type of feeding, respiratory support at 36 weeks’ post-menstrual age (PMA), and infant and maternal demographics. Fenton growth curves or World Health Organization growth curves were used to determine z-scores. Body composition measurements were obtained using bioelectrical impedance analysis (BIA) with the BodyStat Quadscan 4000 within 72 hours preceding discharge; to improve precision, measurement was repeated four times within 10 minutes per infant. The median resistance value from the BIA measurements was used in the Kushner equation to calculate %FFM for each infant. The %FFM in steroid-exposed and non-steroid-exposed cohorts was compared using Mann-Whitney U tests.
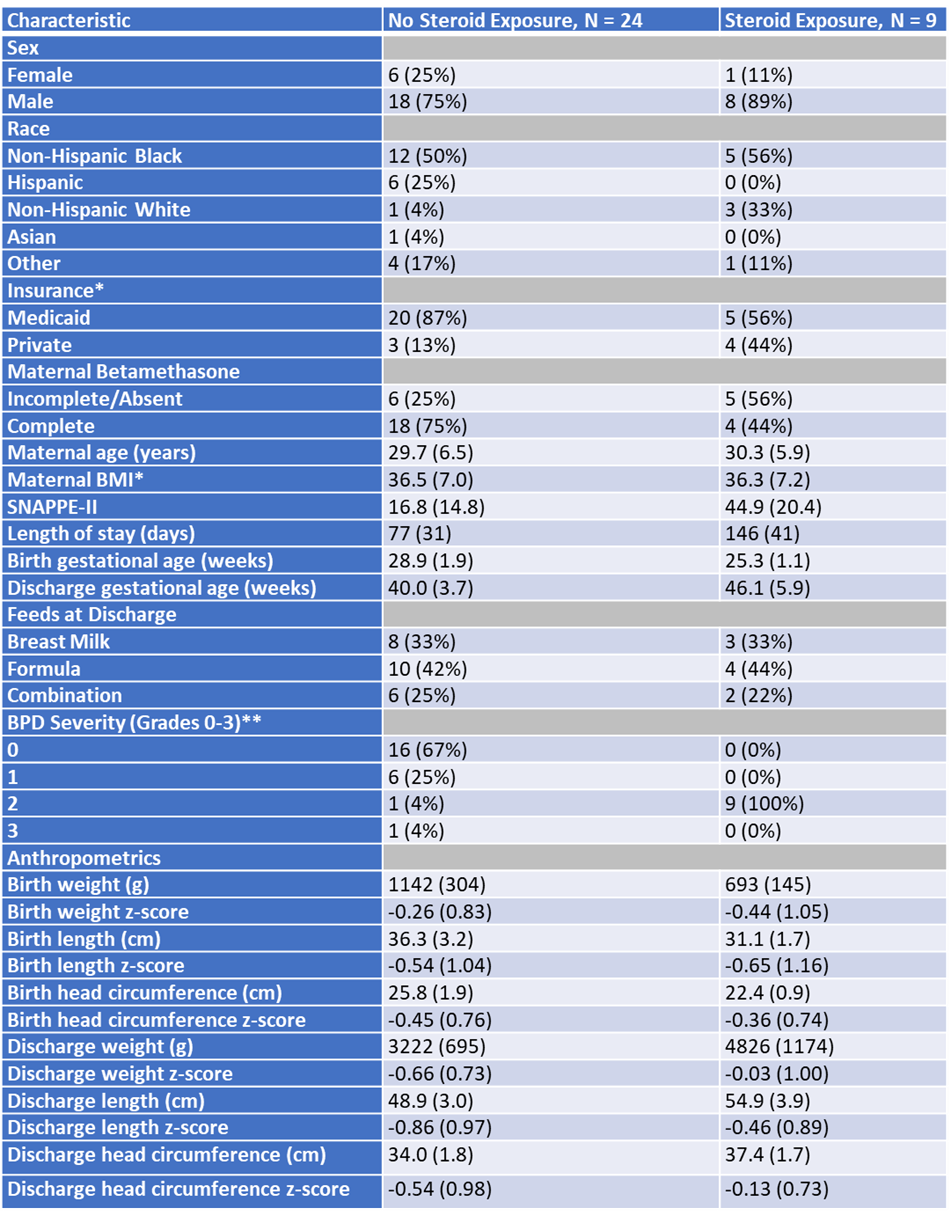
Results: 33 infants (79% male) were enrolled with mean BW 1019 ± 331 g and mean GA 28 ± 2 weeks with 9 (27%) steroid-exposed infants (Table 1). Bivariate analysis demonstrated that %FFM at NICU discharge was lower in the steroid-exposed cohort compared to the non-steroid-exposed cohort (median 74% vs. 91%, p= .043).
Conclusion(s): Steroid exposure, which is usually indicated due to severe BPD, was associated with decreased %FFM. FFM is an important indicator of nutritional status and neurodevelopment among VP infants. Although our preliminary findings cannot determine if this association is due to an independent effect of steroids on FFM accrual or to shared determinants of steroid use and FFM accretion, our data demonstrates increased nutritional risk among steroid-exposed VP infants and supports enhanced surveillance of these infants after discharge.