Quality Improvement/Patient Safety: Improvement Science Research Methods
QI 1: Improvement Science Research Methods & Evaluation of QI Educational Interventions
679 - Importance of Risk Adjusting Central Line-Associated Bloodstream Infection Rates in Children
Publication Number: 679.151
- LS
Lakshmi Srinivasan, MBBS MTR (she/her/hers)
Assistant Professor
CHOP - 3401 Civic Center BlvdPhiladelphia, PA 19104-4319UNI
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background:
Central line-associated bloodstream infection (CLABSI) is the most prevalent pediatric healthcare associated infection Develop a risk adjustment model for CLABSI in hospitalized children and compare crude to adjusted rates to determine the impact of adjusting for patient level factors. , and is frequently used to benchmark performance of pediatric hospitals. Existing approaches to risk adjustment for CLABSI do not control for individual patient characteristics, which are strong predictors of risk of CLABSI and vary greatly within and across pediatric hospitals over time.
Objective:
Design/Methods:
We included hospitalized children with central lines between Jul 1, 2013 and Mar 31, 2022 from a quaternary children’s hospital. ‘Central line days’ and CLABSI events were identified and validated according to National Health Surveillance Network definitions. We extracted data from the electronic health record on patient demographics, comorbidities and line-related factors. We utilized a new construct: receipt of ICU level of care by organ system, regardless of whether patient was in an ICU bed, with severity represented by the need for any ICU level of care, and complexity the number of organs requiring it. Risk factors considered for inclusion in multivariable modeling were based on association with CLABSI risk in univariate modeling (p value< 0.10), multicollinearity, and clinical expert input. Yearly expected CLABSI rates derived from the risk adjustment model were compared to observed CLABSI rates.
Results:
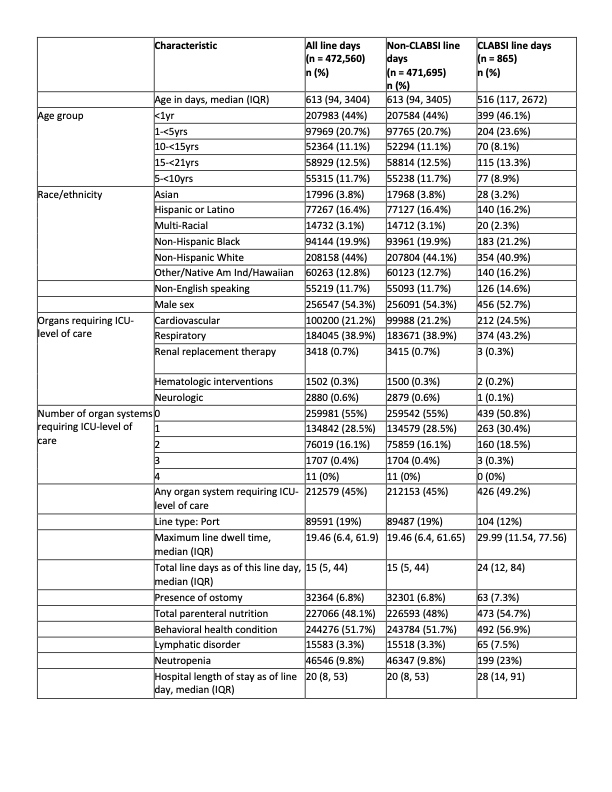
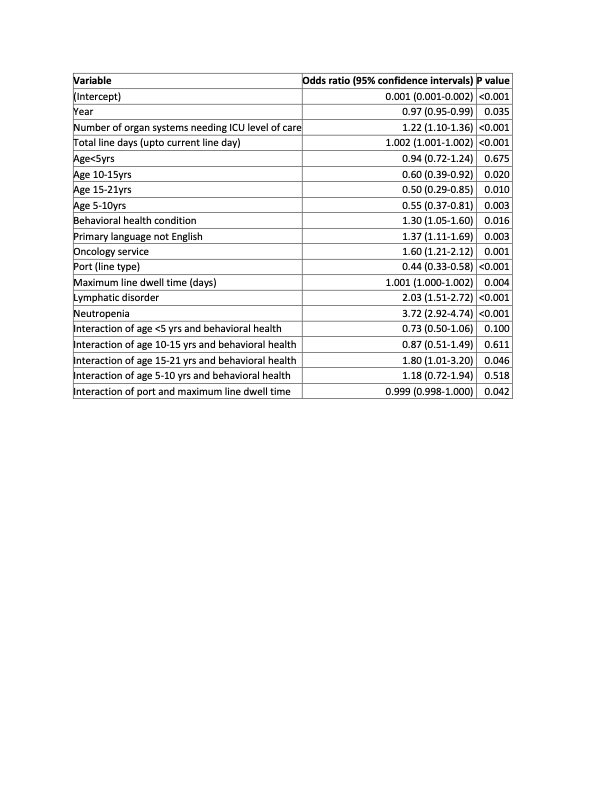
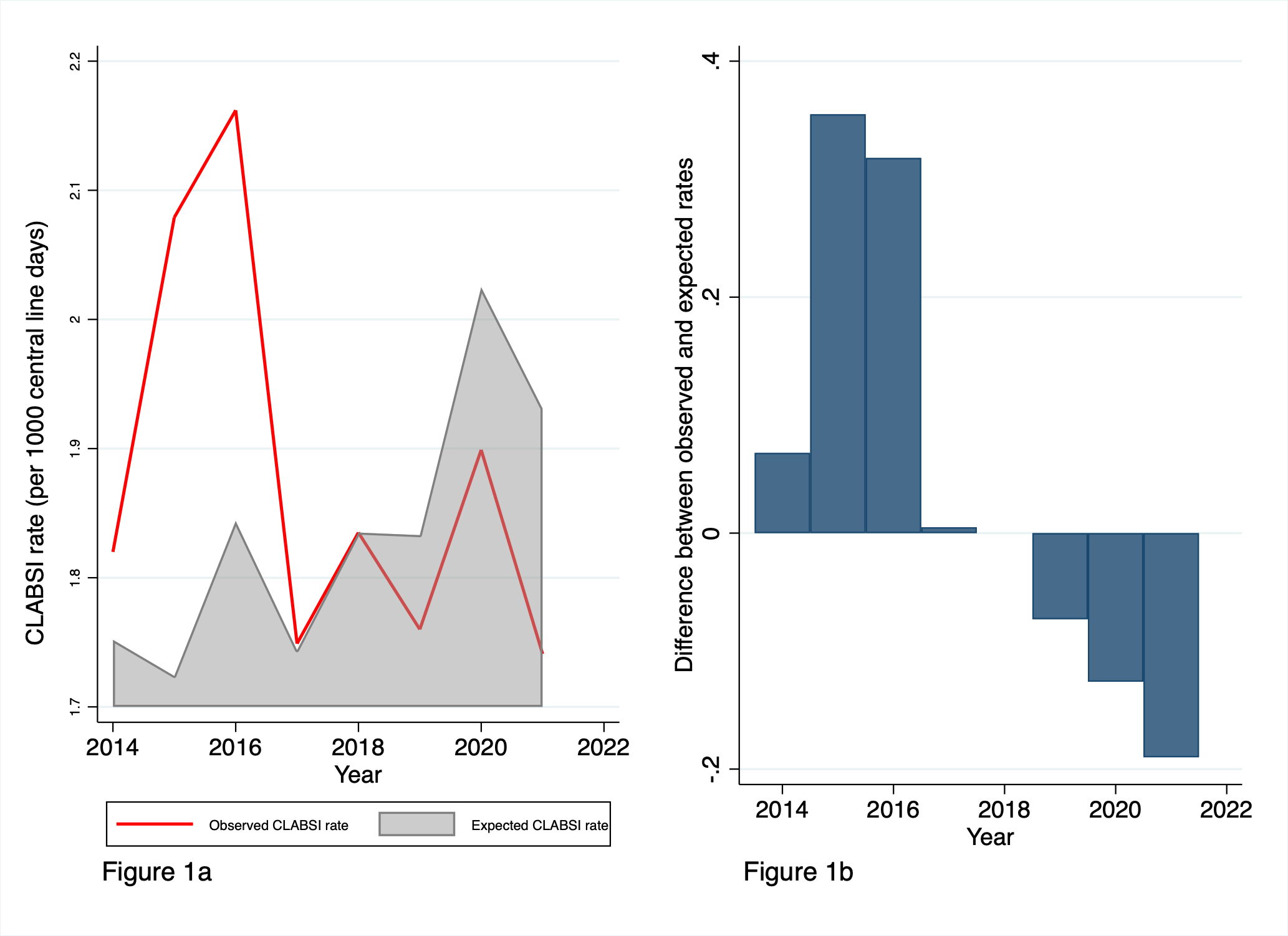
During the study period, 15,166 patients had a total of 472,560 line days. Among these, 680 patients had a total of 865 CLABSIs (Table 1). The final risk adjustment model included total line days, age group, behavioral health condition, non-English speaking, oncology service, port line type, line dwell days, lymphatic disorder, neutropenia and number of organ systems requiring ICU level care (Table 2). For every organ system receiving ICU level of care, there was 1.23 times the odds of CLABSI (95% CI 1.10-1.37). Controlling for patient risk factors, there was a decrease in CLABSI risk over time (OR 0.97/year). Observed rates were lower than the expected rates for recent years, and the differences between the two increased over time (Figure 1a-b).
Conclusion(s):
Failure to adjust for patient factors, particularly severity and complexity of disease, may miss clinically significant differences in CLABSI rates within and across hospitals. Following validation, risk adjustment methods should be used in quality improvement and hospital benchmarking efforts.