Breastfeeding/Human Milk
Breastfeeding/Human Milk 2: Addressing Inequities in Lactation
381 - Improving Breastfeeding Communication Across the Healthcare Continuum: Listening to Latina Women
Publication Number: 381.102

Deanna Nardella, MD (she/her/hers)
Postdoctoral Fellow, National Clinician Scholars Program
Yale School of Medicine
Presenting Author(s)
Background: In the United States, there are persisting racial/ethnic breastfeeding (BF) inequities, including in women’s achievement of their BF goals. For Latina women, communication breakdowns in the context of BF care across the pregnancy and postpartum continuum may contribute to these inequities.
Objective: Explore the lived communication experiences of Latina women in the context of BF care during pregnancy, birth, and postpartum.
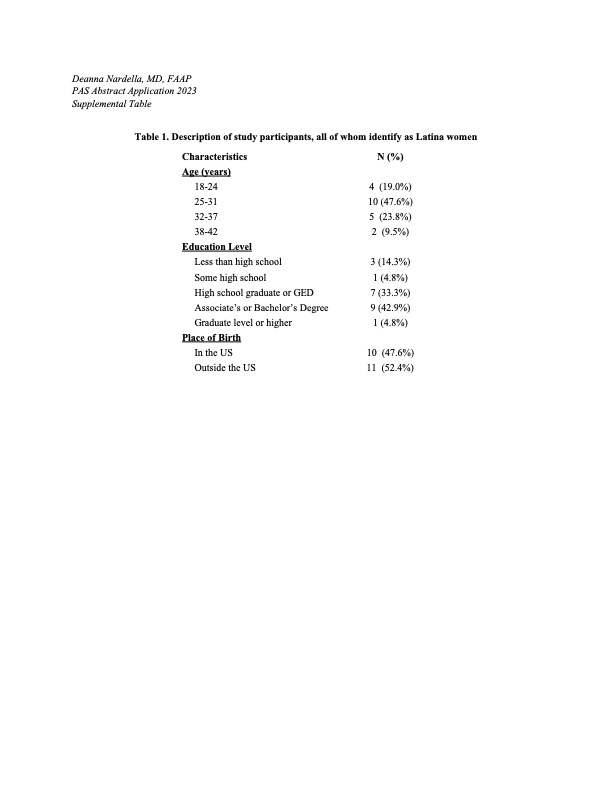
Design/Methods: We conducted a community-engaged qualitative study, interviewing 21 Latina women with low incomes in Connecticut who had breastfed in the last 2 years. Interviews were completed in English and Spanish and elicited information about communication experiences in the context of BF care during the prenatal, perinatal, and postpartum periods, as well as recommendations for improvement. We analyzed data thematically and conducted comparisons by care setting, provider type, and pregnancy period.
Results:
Across providers and care settings, ‘having more respectful communication’ emerged as a priority for women – for example, more use of respectful non-verbal cues (e.g., eye-contact, respectful tone, gentle touch, not rushing) and BF encouragement from the healthcare team. Most women felt the need to self-advocate and self-educate and grew frustrated with inconsistent BF counseling among providers. Often overwhelmed by handouts, women desired culturally appropriate, easily accessible BF information across care settings.
Nurses and lactation counselors and consultants largely led BF conversations across care settings. Women often reported brief, basic BF discussions from obstetric and pediatric providers, preferring open discussion on goals, anticipated or lived challenges, and support. Though women recognized that nurses and doctors may not have the time or expertise for in-depth discussions on BF, they desired improved provider BF knowledge (e.g., latch, building milk supply) and access to lactation counselors and consultants throughout pregnancy and postpartum.
Prenatally, women recommended a visit dedicated to discussing BF benefits, challenges, and plans. Around delivery, women were dissatisfied with verbal guidance on breast pumps, latching, and milk supply. Postpartum, women desired more BF positive reinforcement from both obstetric and pediatric providers.
Conclusion(s): Multilevel interventions tailored to care setting, provider type and pregnancy period are needed to improve the quality of communication in the context of BF care for Latina women, with an emphasis on delivering respectful BF care.