Medical Education: Diversity, Equity & Inclusion
Medical Education 8: Diversity, Equity, & Inclusion 2
569 - Words Matter: Examination of language use in a case of pediatric obesity
Publication Number: 569.23

Jacee L. McCoy, B.S. (she/her/hers)
Medical Student
McGovern Medical School at the University of Texas Health Science Center at Houston
Houston, Texas, United States
Presenting Author(s)
Background:
When healthcare providers discuss their patients’ body weight, their language can positively or negatively affect them. Stigmatizing words can profoundly impact patient health by potentially obstructing care, fostering mistrust, and disseminating bias.
Objective:
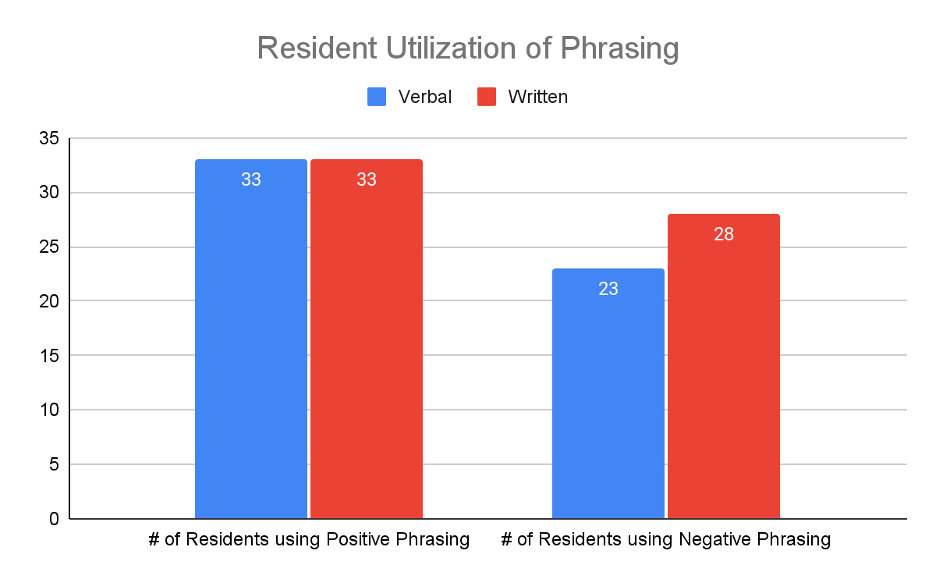
Examine the use of stigmatizing and non-stigmatizing language used by resident physicians managing a pediatric patient with an obesity diagnosis, to determine the educational needs of physicians in their communication with patients. All residents utilized positive phrasing in both forms of communication (Fig. 1). Meanwhile, 23 residents (69.6%) utilized negative verbal phrasing while 28 (84.8%) utilized negative written phrasing (Fig. 1). Common negative terms were “obese”, “overweight”, and “heavy”. Common positive terms were “weight” and “BMI”. The most common positive approach to patient care in the verbal format was bilateral decision making, while patient personalization was prevalent in the written format. Nearly half (18) of the residents utilized a Therapeutic/Emotional approach during the encounter.
Design/Methods: 33 pediatric interns completed an Objective Structured Clinical Examination (OSCE) and patient note with a standardized mother whose daughter was evaluated for obesity and bullying. Encounter videos and post-encounter notes were analyzed for positive (empathetic) and negative (stigmatizing) language. Terms were identified using the mindful language toolkit from Stanford University School of Medicine Words Matterworkshop as well as in-depth PubMed searches. Example stigmatizing words included "obese" and "large" and non-stigmatizing terms included "BMI" and "weight”. Positive approaches to patient care were documented if providers were approving, personalizing the patient, or promoting bilateral decision making. Encounters were further categorized as either: 1. Therapeutic/Emotional: when the focus was on the patient’s mental health and school bullying; 2. Medical: when the focus was the patient’s physical health and weight; or 3. Mixed: equal time focusing on the patient’s mental and physical health.
Results:
Conclusion(s):
The high use of negative phrases illustrates a need for physician education that may or may not be limited to our residency program. Physicians’ words can affect children’s health, development, provider relationship, and outlook on the healthcare system. We hope to bring awareness to this problem as implicit biases can impose a detriment to our patients, especially as obesity in the pediatric population is on the rise and the 21st Century Cures Act provides complete access to the medical record.