Medical Education: Simulation & Technology
Medical Education 6: Simulation & Technology 1
539 - Use of Electronic Text Messaging of Neonatal Resuscitation Program Principles to Pediatric Residents and Impact on Knowledge Retention
Publication Number: 539.228

Kathleen Tedesco, MD (she/her/hers)
Resident PGY3
LAC+USC Medical Center/Keck School of Medicine of the University of Southern California
Los Angeles, California, United States
Presenting Author(s)
Background:
Pediatric residents have limited exposure and opportunities to master skills needed to resuscitate newborns.
Objective:
The purpose of this study was to provide learning via text messaging of Neonatal Resuscitation Program (NRP) 8th edition principles and assess retention and integration of skills.
Design/Methods:
This was a randomized controlled, prospective study including Pediatrics and Medicine-Pediatrics residents at a level 3 Neonatal Intensive Care Unit (NICU). Thirty participants were randomized using Excel features into a control group, receiving no text messages, and an intervention group, receiving biweekly NRP content pearls (Image 1) for 6-weeks. An initial survey and quiz assessed baseline confidence and knowledge in neonatal resuscitation, followed by text messages sent to the intervention group over 6-weeks. All participants took a quiz at the end. This was followed by a 6-week period of no contact, then a quiz at the end of 12-weeks. The study concluded with two high fidelity simulations, a term infant with abruption (scenario 1) and a preterm infant (scenario 2) scored using a validated tool to assess integration of skills. Data was analyzed using SPSS software.
Results:
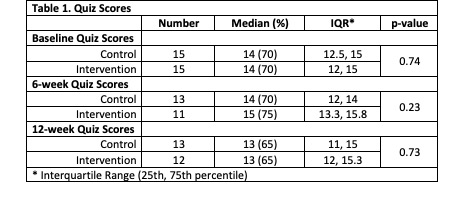
Of the 30 participants, 24 were Pediatric residents and 6 were Medicine-Pediatrics residents. Forty-seven percent were PGY-1. Seventy percent had attended less than 6 resuscitations of infants. Eighty percent of the control group and 53% of the intervention group had a NICU rotation during the study. Most agreed they needed more knowledge and experience in neonatal resuscitation. There was no difference in quiz scores between groups (Table 1). The intervention group scored significantly higher in scenario 1, and both groups scored similarly in scenario 2 (Table 2). Breakdown of the simulations showed the intervention group did significantly better with chest compressions (p-value 0.003) and epinephrine/volume administration (p-value 0.028). The final survey showed both groups still feel they need more knowledge and experience with neonatal resuscitation; however, the intervention group had increased confidence in leading a resuscitation.
Conclusion(s):
Despite similar quiz scores between groups, the intervention group experienced an increase in confidence in leading a neonatal resuscitation. Additionally, the intervention group scored better in the simulation of scenario 1, specifically on chest compressions and epinephrine/volume administration. Future plans include repeating the study with a larger group, adjusting the time, frequency, and length of texts, and using multi-media pearls such as audio or video..jpg)
.png)
