Breastfeeding/Human Milk
Breastfeeding/Human Milk 2: Addressing Inequities in Lactation
380 - Initial Feeding Method, WIC-Provided Lactation Support, and Breastfeeding Duration at an Urban Pediatric Primary Care Practice
Publication Number: 380.102

Alana Engelbrecht, B.S. (she/her/hers)
Medical Student
State University of New York Downstate Medical Center College of Medicine
Pleasantville, New York, United States
Presenting Author(s)
Background:
Breastfeeding (BF) is associated with improved maternal and infant health outcomes. However, access to lactation support is limited for underserved populations. In our urban pediatric primary care practice (PPCP), we partnered with our local WIC office to integrate a WIC peer counselor (trained lactation counselor) to provide lactation support for our newborn visits.
Objective:
We aimed to study the association of BF duration with 1) a WIC peer counselor integrated pediatrics visit and 2) initial feeding methods.
Design/Methods:
This is a retrospective cohort study using a chart review of a convenience sample of patients from our PPCP who met with a WIC-provided lactation counselor (WPLC) compared with a matched cohort that did not. Patients were matched based on race, ethnicity, and insurance using a greedy matching algorithm. Chi-square was used to compare across initial infant feeding methods as documented at the infant’s first PPCP visit. Duration of any BF and exclusive BF was compared across groups using a t-test. ANOVA (f-test) was used to compare these variables across initial feeding methods.
Results:
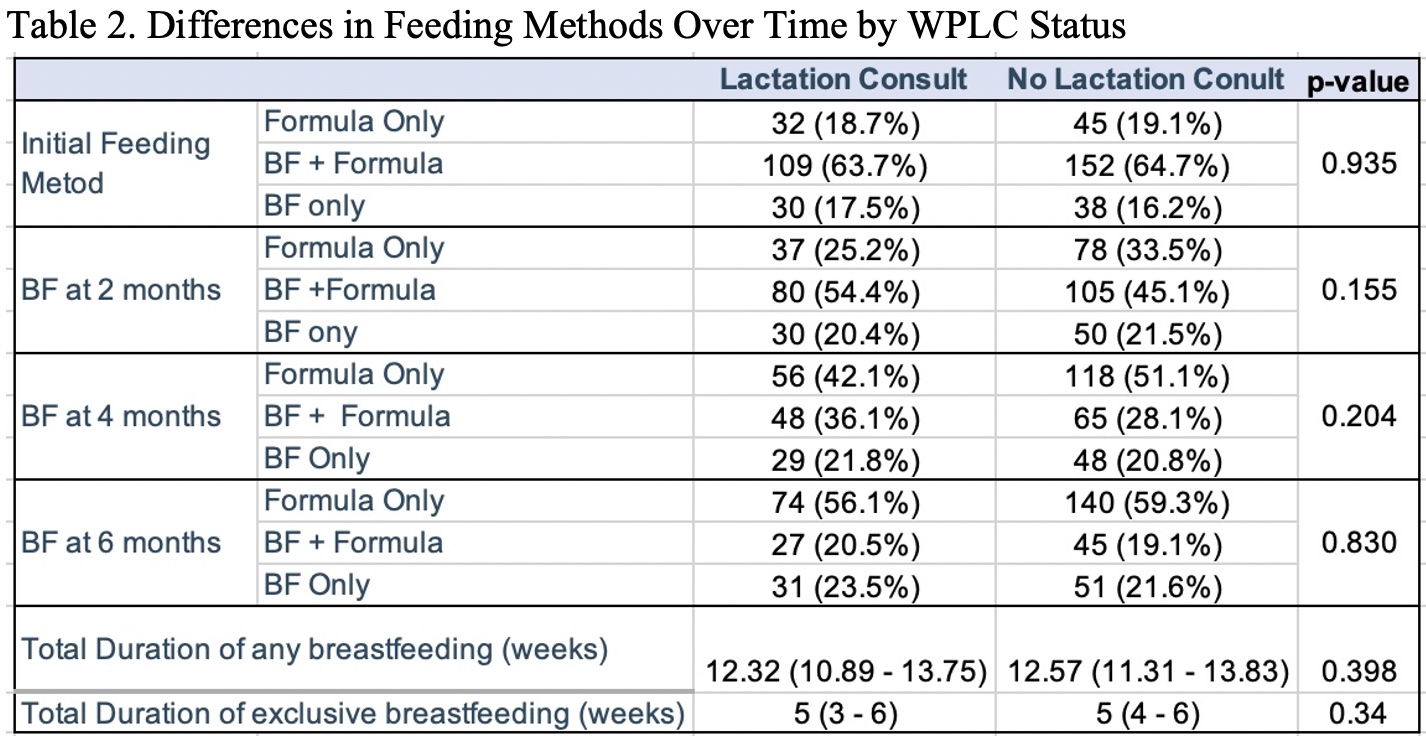
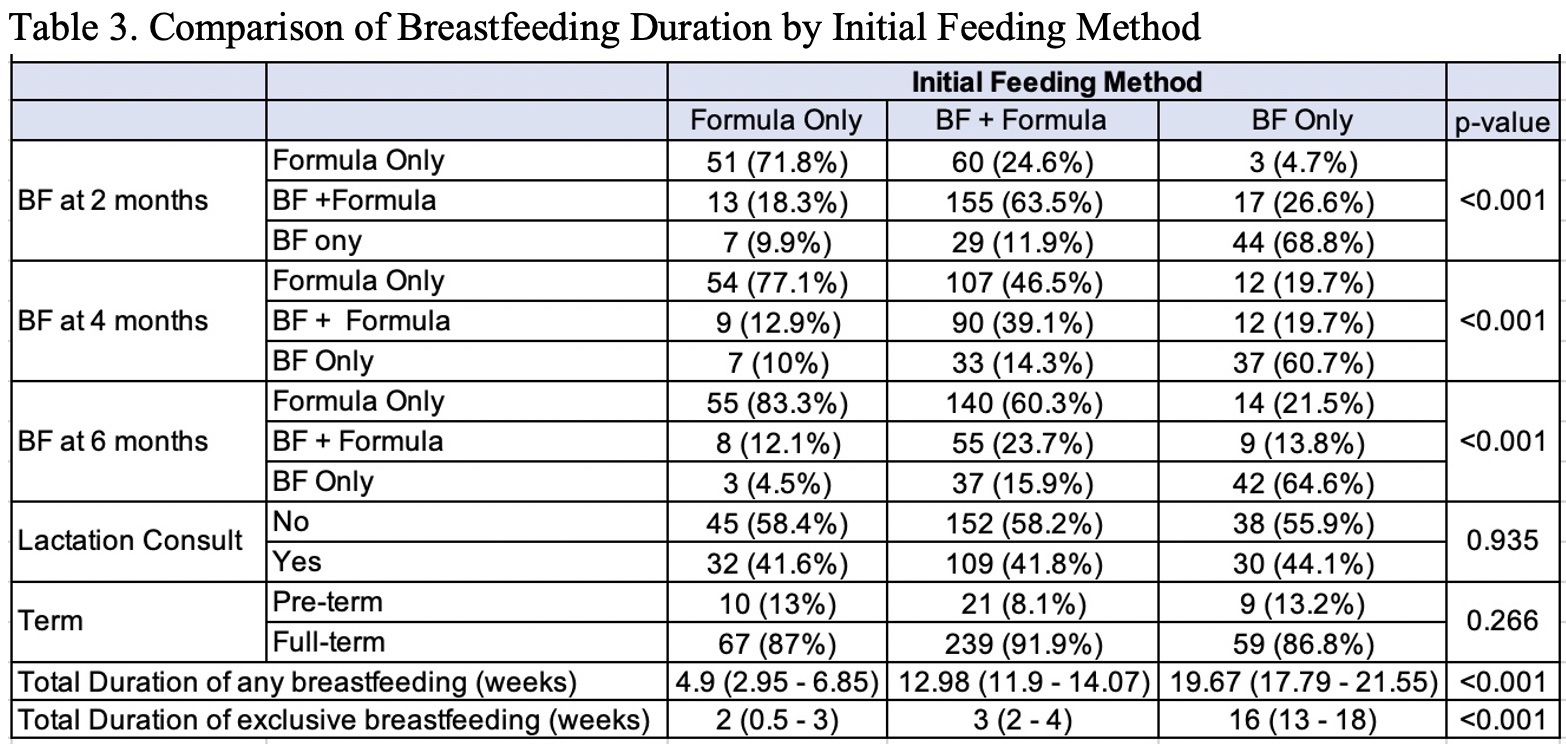
A cohort of 111 infant mother dyads that received WPLC from July 2019 to April 2022 were matched to 222 pairs that did not receive WPLC. Our study population included 21% (69/333) non-English language speakers, 41% (136/333) Hispanic families, and 91% (303/333) receiving Medicaid (Table 1). There was no significant difference in feeding methods between those who did and did not receive WPLC (Table 2). Compared to infants whose initial feeding method was exclusive BF, fewer infants who used formula or both formula and breastmilk as initial feeding methods were exclusively BF at the respective 2-month (68.8%, 9.9%, 11.9%), 4-month (60.7%, 10%, 14.3%), and 6-month visits (64.6%, 4.5%, 15.9%) (p< 0.001) (Table 3). There was a significant association found for initial feeding method and total duration of any BF (Formula only: 5 weeks; BF and Formula: 13 weeks; Exclusive BF: 20 weeks, p< 0.001) and for total duration of exclusive BF (Formula only: 2 weeks; BF and Formula: 3 weeks; Exclusive BF: 16 weeks, p< 0.001) (Table 3).
Conclusion(s):
There was no association between integrated WPLC and BF duration in our cohort. However, there was a significant association between initial feeding method and BF duration. Future studies should explore whether prenatal lactation support encouraging early and exclusive BF would bolster BF duration..jpg)