Neonatal-Perinatal Health Care Delivery: Practices and Procedures
Neonatal-Perinatal Health Care Delivery 2: Epi/HSR Equity
635 - Parent Factors Associated with Neonatal Intensive Care Unit (NICU) Discharge Readiness in High-Risk Infants
Publication Number: 635.141
.jpg)
Kelsey R. Anderson, MD (she/her/hers)
Fellow
McGovern Medical School at the University of Texas Health Science Center at Houston
Houston, Texas, United States
Presenting Author(s)
Background:
Lessening the burden of neonatal healthcare costs for families and hospitals is warranted as preterm births increase worldwide. Ensuring parents are ready to successfully transition home from the NICU with their infants may reduce the burden of unplanned healthcare resources, especially for medically complex infants. The American Academy of Pediatrics and the National Perinatal Association published policy statements to guide clinicians preparing infants and families for NICU discharge; however, the specific parent readiness factors that predict successful transition home is not clear.
Objective: The primary aim is to determine the parent-centered measures and factors of discharge readiness that predict successful transition home for medically complex NICU infants.
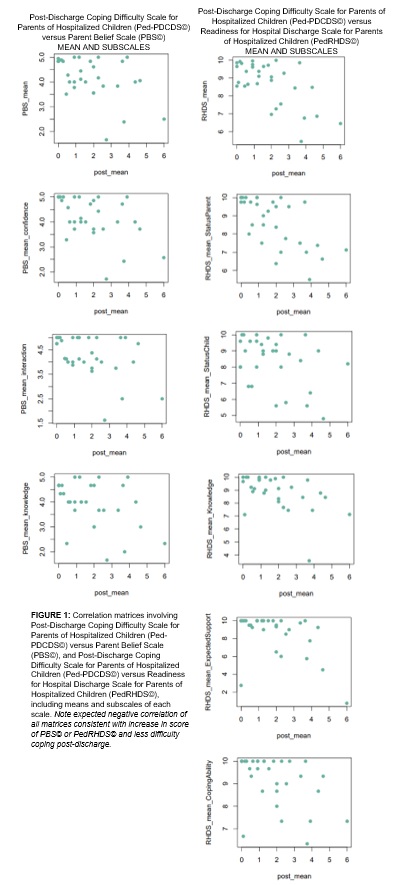
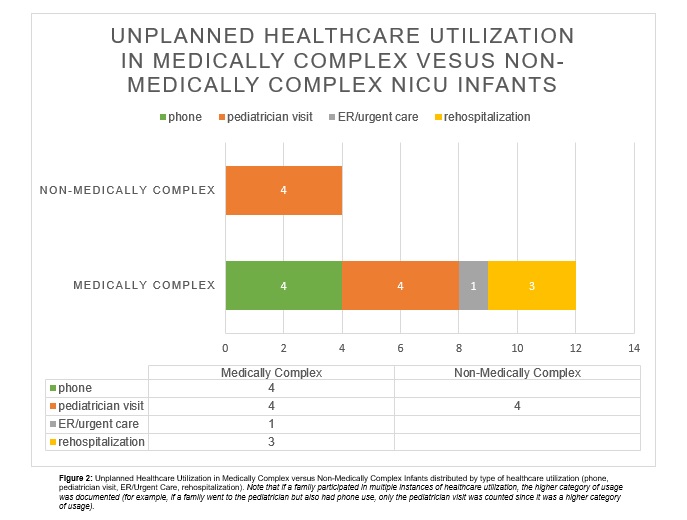
Design/Methods: A descriptive, longitudinal pilot study of 122 parent-dyads was performed to examine parent-centered factors associated with readiness for NICU discharge and successful transitioning of their infant home. Parent readiness factors, such as confidence, knowledge, support, and coping were evaluated at time of discharge and one-month post-discharge using PedRHDS©, PBS©, and Ped-PDCDS© along with additional factors determined from the literature. Assessments of parent readiness were also completed by the discharging attending physician and nurse. Successful transition home from the NICU was measured by parent reports of unplanned healthcare use and parent coping score on the Ped-PDCDS©. Statistical analysis was done using paired t-tests for group comparisons and univariable linear regression for predicting outcomes.
Results: Of the 122 dyads enrolled to date, 90 completed the survey administered at discharge and 37 completed the survey administered one-month post-discharge (response rate = 41%). At discharge, 36% of parents had concerns about going home with their infant and only one parent reported that they were not ready for discharge at one month. Parents reporting high readiness for discharge had less difficulty coping at one-month post-discharge (Figure 1). Infants categorized as medically complex had higher rates of healthcare utilization at one-month post-discharge with 4 out of 21 infants requiring potentially avoidable healthcare utilization, such as ER/urgent care and rehospitalization (Figure 2).
Conclusion(s):
The use of validated assessment tools at the time discharge may identify specific areas to improve parents’ readiness for discharge as well as evaluate a NICU discharge program, especially for medically complex infants.