Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 8
568 - Health-Related Social Risks Among Caregivers of Hospitalized Infants
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 568
Publication Number: 568.412
Publication Number: 568.412
Pyone David, Comer Children's Hospital at University of Chicago Medical Center, Chicago, IL, United States; Victoria Winslow, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Chicago, IL, United States; Jyotsna S.. Jagai, University of Chicago, Chicago, IL, United States; Emily M. Abramsohn, University of Chicago, Chicago, IL, United States; Walid Hussain, University of, Chicago, IL, United States; ANDREW Franklin, NorthShore University HealthSystem, Evanston, IL, United States; Christine Omalley, The university of chicago, Chicago, IL, United States; Stacy Lindau, University of Chicago, Chicago, IL, United States
Pyone David, MD, MSW (she/her/hers)
Neonatology Fellow
Comer Children's Hospital at University of Chicago Medical Center
Chicago, Illinois, United States
Presenting Author(s)
Background: Health-related social risks (HRSRs) are associated with preterm birth, neonatal intensive care unit (NICU) admission, and adverse childhood outcomes. NICU admissions are associated with medical complexities and caregiver stress in the early postpartum period. CommunityRx-Hunger (CRx-H), a randomized clinical trial utilizing a hospital-based community resource referral intervention, focuses on alleviating HRSRs among hospitalized children's caregivers at an urban children’s hospital located in Chicago, Illinois.
Objective: To compare baseline rates of HRSRs in caregivers of infants admitted to NICU versus non-NICU settings.
Design/Methods: A cross-sectional descriptive analysis of baseline and one-week data from the CRx-H RCT evaluated FI and other HRSRs among caregivers of hospitalized children. This study is limited to caregivers of children < 1 year of age (n=183). FI was measured using the USDA U.S. Household Food Security Scale. Inclusion criteria for the caregiver included being >18 years old, a native English or Spanish speaker, living in 1 of 42 targeted ZIP codes, self-identifying as a primary caregiver of the hospitalized child, and an expected hospital stay of >24 hours to < 30 days for the child.
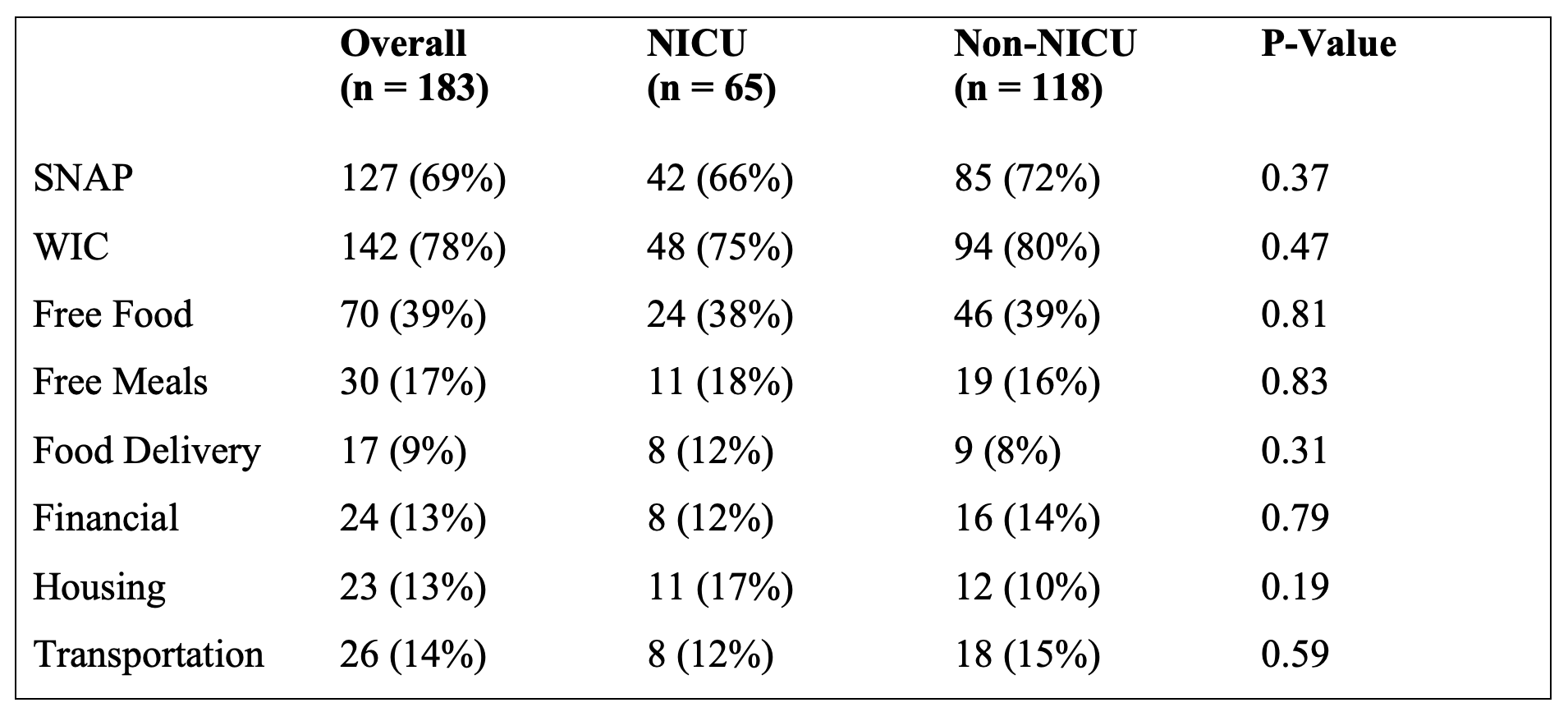
Bivariate analyses compared caregiver sociodemographic characteristics, participation in food assistance resources (SNAP/WIC), and HRSRs (food security, housing, safety, utilities, and transportation) by NICU versus non-NICU admission group for hospitalized infants < 1 year of age.
Results: Most caregivers (NICU, n=65; non-NICU, n=118) were the mother of the hospitalized child (97%), non-Hispanic African American/Black (79%), Medicare/Medicaid recipients (78%), and had a household income < $50,000 (82%) (Table 1). Although caregivers of children in the NICU were more likely to be ≥30 years old (p = 0.01), partnered (p = 0.02), and have at least some college education (p=0.03) (Table 1), the rate of 30-day food insecurity was similar among the two groups (29% of NICU vs 31% of non-NICU) (Figure 1). More than half screened positive for at least one HRSR (54% of NICU vs 55% of non-NICU) and ≥78% participated in assistance resources (no significant differences by group, Table 2). Caregivers utilizing WIC were more likely to have FI over the previous 30 days compared to those not using WIC (p=0.02).
Conclusion(s): Parents of infants hospitalized in the NICU had higher socioeconomic status than, but equivalent rates of HRSRs as, parents of infants in other hospital units. These findings suggest that NICU hospitalization may confer unique financial stress or other barriers to meeting basic material needs.
.png)
.png)
