Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 5
445 - Community versus vertically acquired neonatal SARS-CoV-2 infection: the EPICENTRE cohort study
Publication Number: 445.431

Daniele De Luca, MD, PhD (he/him/his)
Full Professor
Paris Saclay
Paris, Ile-de-France, France
Presenting Author(s)
Background:
Neonatal SARS-CoV-2 infection is uncommon although it can be life-threatening. SARS-CoV-2 can infect neonates either from the environment (community-acquired; CA), or from the pregnant mother in utero through the placenta or peripartum during the delivery (vertically-acquired; VA). Due to the low numbers of reported neonatal SARS-CoV-2 infections, it is unknown whether CA and VA have different clinical characteristics.
Objective:
We aimed to examine the clinical features of CA and VA neonatal SARS-CoV-2 infections reported in the EPICENTRE (EsPnIC Covid-19 paEdiatric NeonaTal REgistry), a prospective, hospital-based, observational registry of pediatric/neonatal SARS-CoV-2 infected-neonates needing hospital care in 13 sites in 10 countries (Europe, Brazil, Middle East and USA).
Design/Methods:
Deidentified data were collected between 17 March 2020 and 20 October 2021 (data lock-out for verification) in a customized REDCap® database for neonates: 1) born to mothers with SARS-CoV-2 infection during pregnancy if they fulfilled the WHO criteria for a VA-infection, and 2) admitted in the first 30 days after birth with proven SARS-CoV-2 infection, if they fulfilled the WHO criteria for a CA-infection.
Results:
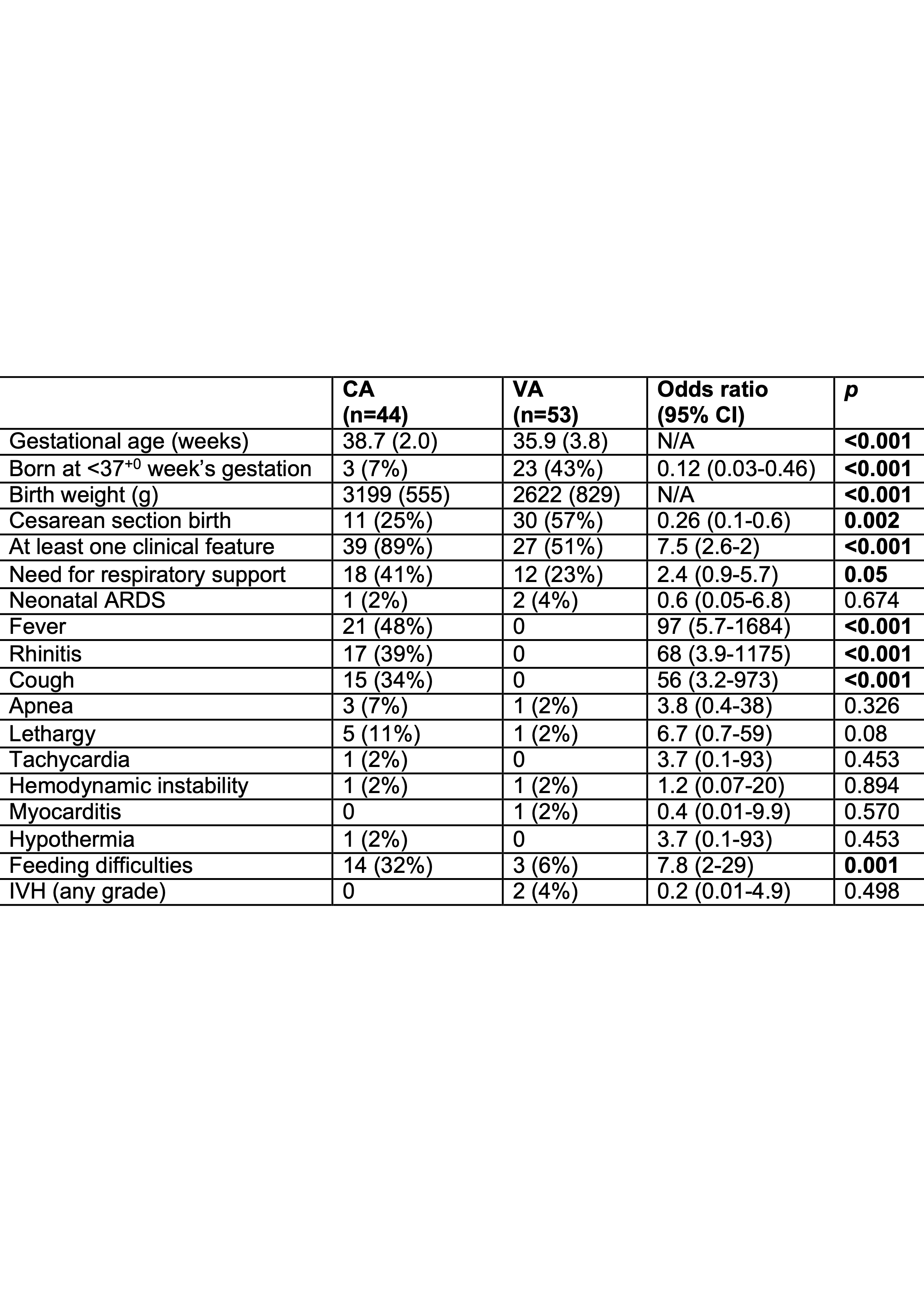
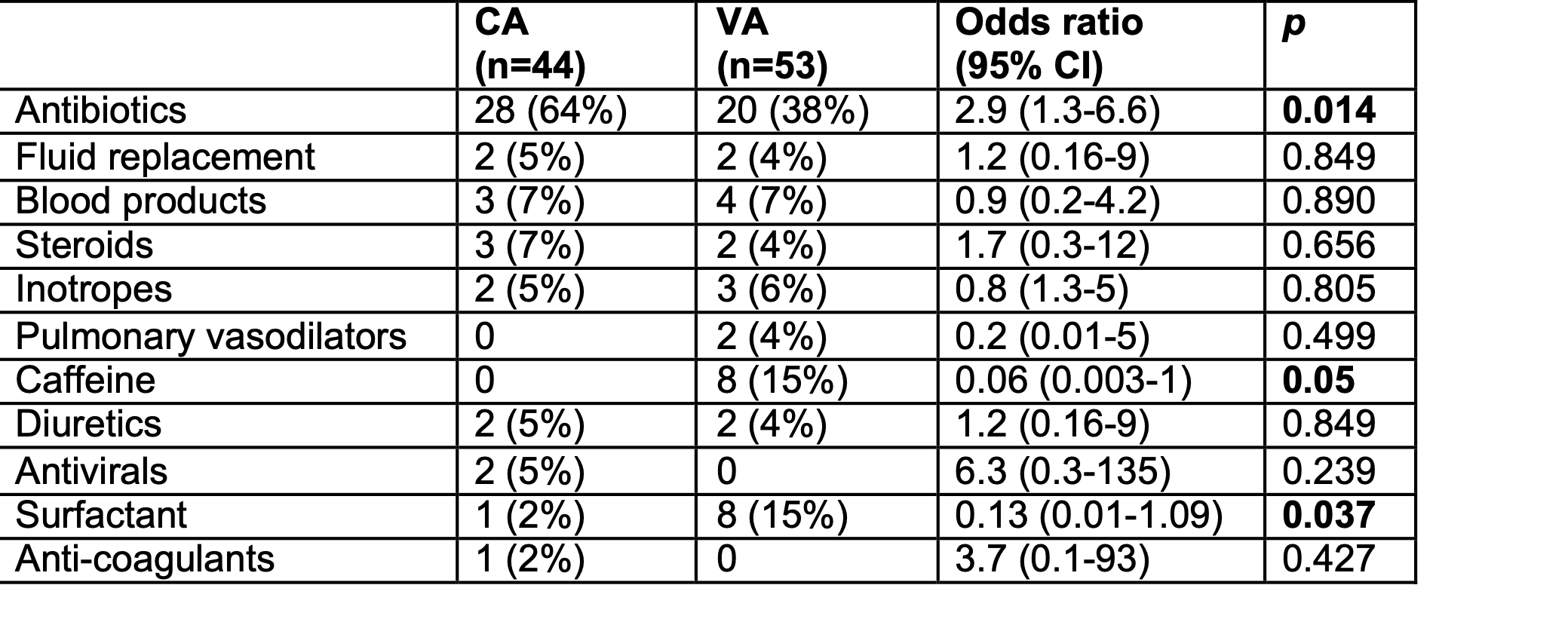
Fifty-three VA and 44 CA infections were identified. VA cases accounted for 7.7% of maternal SARS-CoV-2 infection (692 mother-baby dyads). The two cohorts were similar, except for lower gestational age and higher cesarean section rate in the VA group (Table 1). All VA infections were detected during the birth admission. Mean (standard deviation) age at the hospital admission of CA cases was 14.7 (8.1) days and 26 (59%) had at least one SARS-CoV-2 positive cohabitor. CA cases had more clinical features (fever, respiratory signs and feeding difficulties; Table 1) which were almost never present in VA cases; two had pediatric inflammatory multisystem syndrome. More CA cases received antibiotics, while drugs used in perinatal care (caffeine, surfactant) were more common in VA cases; two CA cases received antivirals (one oseltamivir and one remdesivir; Table 2). Extracorporeal life support was never used; one VA patient died from causes unrelated to the infection. Median [interquartile range] hospital stay was similar in CA (8 [3-14]) and VA (8 [5-25] days) cases.
Conclusion(s):
CA cases who need hospitalization have more clinical features than VA cases.