Adolescent Medicine: Disordered Eating
Adolescent Medicine 3
514 - Relationship between insurance type and inpatient hospitalization and ambulatory visits for adolescents with eating disorders during the COVID-19 pandemic
Publication Number: 514.3

Morgan Chojnacki, DNP, CPNP-PC, APRN (she/her/hers)
Assistant Professor
Kentucky Children's Hospital University of Kentucky College of Nursing
Lexington, Kentucky, United States
Presenting Author(s)
Background:
Hospitalization for medical stabilization of patients with eating disorders (EDs) occurs when EDs are not stable, and should be followed by residential or intensive ambulatory care settings. Repetitive medical hospitalization without subsequent intensive outpatient or residential treatment may not meet ED patients’ needs for psychological and physical rehabilitation. Medical insurance type may affect the rate of ED instability and hospitalization.
Objective:
The current study aims to identify the relationship between insurance type and rate of hospitalization for medical stabilization of EDs and ambulatory visits in adolescents before and during the COVID-19 pandemic. Associations between insurance status and level of care during the pandemic were also evaluated.
Design/Methods:
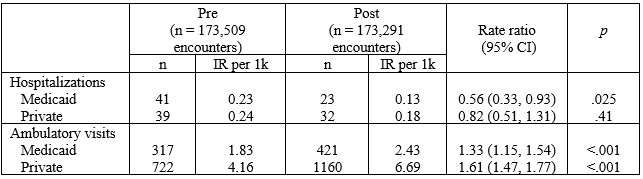
Data extraction from electronic medical records at Kentucky Children’s Hospital of adolescents 9-17 years old with ambulatory or medical hospitalization associated with ED diagnosis was performed. Diagnoses included anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder (BED), and unspecified eating disorder. Incident rate ratios were used to evaluate changes in the rate of encounters over time: Pre-COVID 19 onset in Kentucky January 1, 2019 – February 28, 2020 and during the pandemic March 1, 2020 – June 30, 2021. Odds ratios summarized the association between insurance status and hospitalization.
Results:
A 44% reduction in the rate of hospitalization for patients with Medicaid during the COVID-19 pandemic occurred, compared to the 13 months prior (IRR = 0.56, p< .001). The rate of ambulatory visits for patients with private and Medicaid insurance increased significantly by 61% and 30%, respectively, in this time frame (both p’s < .001). During the pandemic, 5.2% of Medicaid ED patient encounters were hospitalizations, compared to 2.7% of those with private insurance; suggesting ED Medicaid patients were nearly 2 times more likely to be hospitalized than ED privately insured patients (OR = 1.98, p = .013).
Conclusion(s): Though patients with private insurance consisted of a larger percentage of adolescent ED ambulatory visits (72%), patients with Medicaid were nearly two times more likely to experience hospitalization for ED than those with private insurance. Further studies should explore eliminating barriers for adolescent patients with EDs and Medicaid insurance that deter treatment outside of the hospital..jpg)