Adolescent Medicine: General
Adolescent Medicine 1
445 - IIncidence of pregnancy according to birth control method usage patterns among adolescent and young adult family planning patients at an urban community pediatric clinic, a retrospective cohort study
Publication Number: 445.1

Sophie H. Allende-Richter, MD (she/her/hers)
Staff Physician
Boston Children's Hospital
Newton, Massachusetts, United States
Presenting Author(s)
Background:
Despite steady decreases in adolescent pregnancy, low-income, minority women continue to be disproportionately affected, facing a higher risk of physical and mental health burdens. Our clinic, a Title X-funded community pediatrics practice allows provides free and confidential reproductive health services. The majority of patients are Latino immigrants and most qualify for public health insurance.
Objective:
To investigate the incidence of pregnancy according to birth control method (BCM) usage patterns among family planning (FP) patients at our clinic to identify areas of improvement in our FP counseling.
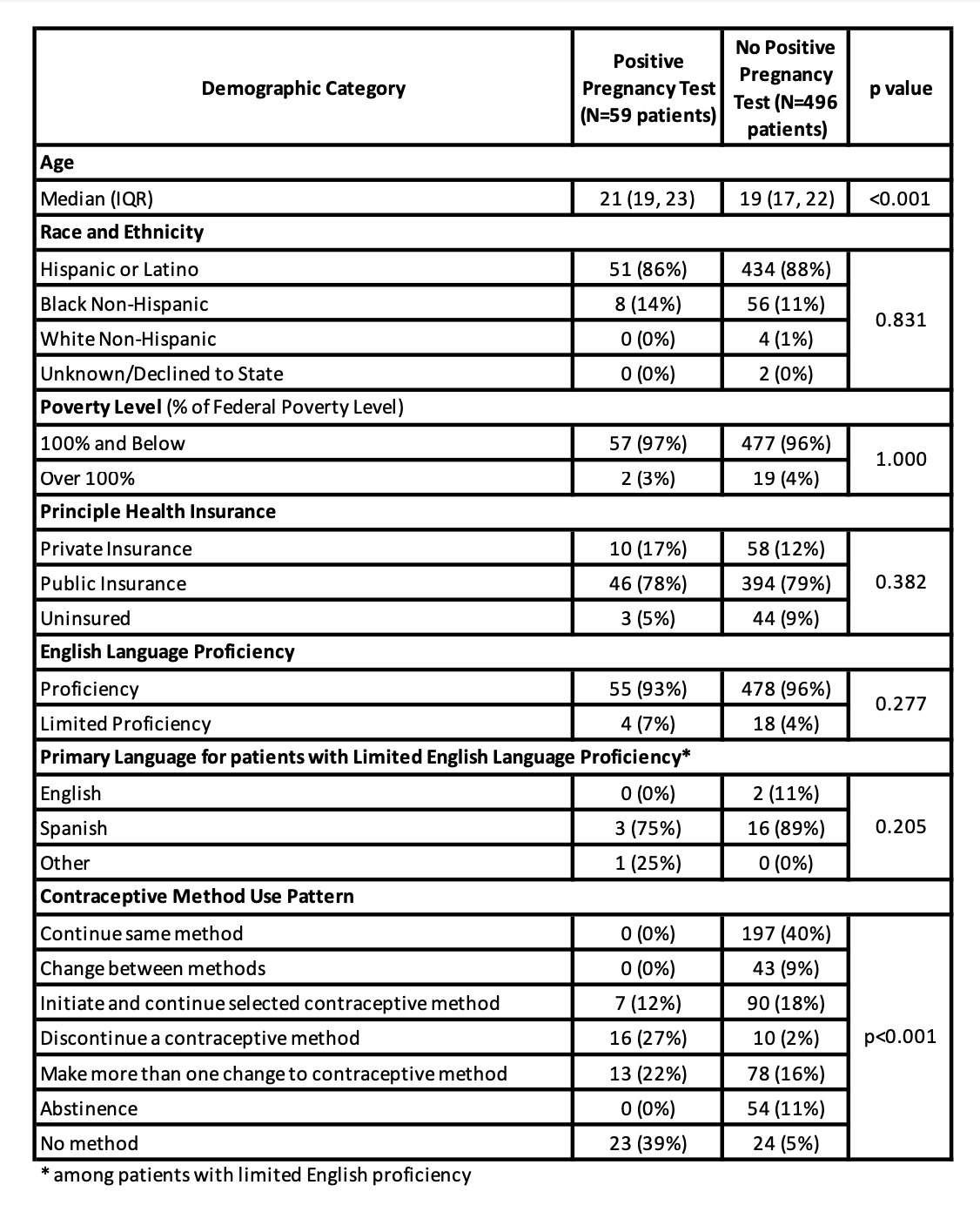
Design/Methods: We conducted a single cohort retrospective chart review of self-identified females aged 12-26 who had at least one FP visit between May 1, 2016 – April 30, 2017. The exposure was BCM usage; the primary outcome was pregnancy incidence within the 12-month period. We performed chi-square and Fisher’s exact tests to analyze the incidence of pregnancy according to patient characteristics and BCM usage patterns. To gauge unplanned pregnancy frequency, we conducted a voluntary survey of FP patients who presented to clinic from June-July 2017
Results:
From May 1, 2016 – April 30, 2017, 555 patients completed an FP visit. Median age was 19; 87% identified as Hispanic and 12% identified as Black Non-Hispanic. BCM usage patterns included: continuing the same BCM, changing between BCMs, initiating a BCM, discontinuing a BCM, no method, abstinence, and making more than one BCM change. Of the cohort, 59 (11%) experienced pregnancy during the period of interest: 23 (39%) had no BCM, 16 (27%) discontinued a BCM, and 13 (22%) made more than one change to their BCM. Pregnancy was significantly associated with these BCM usage patterns (p < 0.001). Of the 555 patients, 5% discontinued their BCM (N=26). Of this group, 69% and 31% discontinued a short-acting (SARC) or long-acting (LARC) reversible method, respectively, with no significant difference in pregnancy frequency based on SARC vs. LARC discontinuation (p=1.000). Fifty FP patients completed our survey; 20 respondents had experienced pregnancy, 15 (75%) had unplanned pregnancies.
Conclusion(s):
Our findings suggest that more BCM changes increases risk of periods without BCM coverage. This may explain why despite free FP services, our clinic has a high pregnancy rate compared to the general adolescent population, irrespective of LARC or SARC usage. BCM changes may be due to method side effects; therefore, increasing patient BCM education and satisfaction could decrease the risk of inconsistent BCM usage and frequent changes.