Critical Care
Critical Care 4
724 - Characterizing Mismatches Between Sepsis Scores and Sepsis Best Practice Alerts in a Pediatric ICU Sepsis Predictive Model
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 724
Publication Number: 724.401
Publication Number: 724.401
Maryam Gilpatrick, Baylor College of Medicine, HOUSTON, TX, United States; Curtis E. Kennedy, Baylor College of Medicine, Houston, TX, United States

Maryam Gilpatrick, MD (she/her/hers)
Pediatric Critical Care Fellow
Baylor College of Medicine
HOUSTON, Texas, United States
Presenting Author(s)
Background: Pediatric sepsis is common with a point prevalence of 8% and up to 25% mortality rate in severe sepsis. Early recognition of sepsis through predictive strategies, including scoring tools, is thought to help reduce sepsis related mortality. The use of automated tools has led to improved recognition and treatment of severe sepsis in pediatric emergency departments (ED) and pediatric intensive care units (PICU). These tools, however, vary greatly between institutions as there is a paucity of evidence supporting a standardized screening tool. Our hospital’s PICU sepsis scoring tool is a multi-variable diagnostic predictive model embedded in our electronic health record. There are both PICU and non-PICU types of sepsis scores and sepsis best practice alerts (BPA) and is it unclear if intended PICU scores are leading to the intended BPA type.
Objective: The purpose of this study is to assess the apparent function of the current pediatric ICU sepsis predictive model in a cohort of PICU patients compared to its designed function.
Design/Methods: Retrospective cohort analysis of pediatric patients admitted to the PICU who were admitted to our hospital and triggered a BPA on or after 1/1/2021 and discharged before 1/1/2022. Subjects were identified using the Electronic Data Warehouse. Designed function is defined by intended model inputs (PICU sepsis scores) and intended model outputs (PICU sepsis BPA). We performed a qualitative analysis to derive PICU and non-PICU sepsis scores and PICU and non-PICU sepsis BPAs.
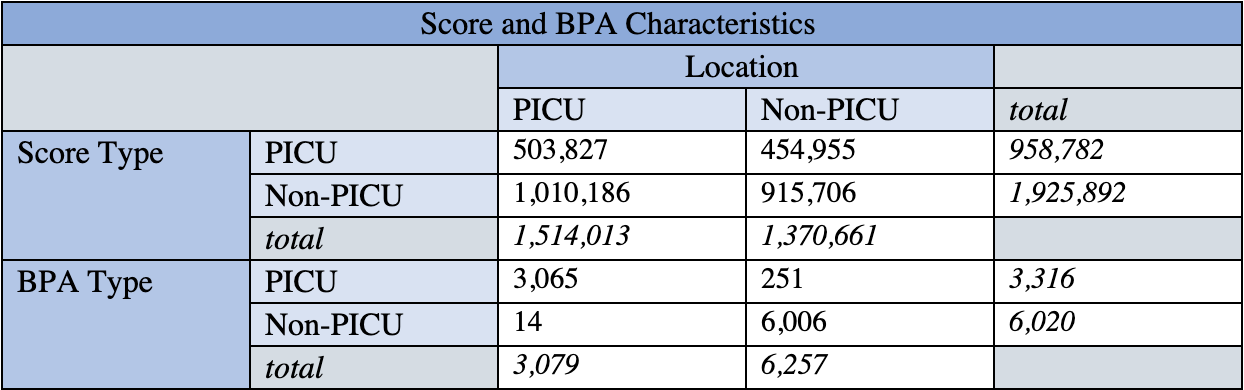
Results: The cohort consisted of 3,058 patients who triggered a BPA. 1,096 (36%) triggered a BPA in the PICU. While in the PICU, 845 (77%) triggered a PICU BPA and 251 (23%) triggered a non-PICU BPA. There were 9,336 total sepsis BPAs and 2,884,674 total sepsis scores. Within the PICU, 3,065 (99%) BPAs were PICU types and 503,827 (33%) scores were PICU types. Overall, 1,419,533 (49%) scores and 9071 (97%) BPAs matched the geographic location of the patient.
Conclusion(s): The ICU sepsis scoring tool is not functioning within its intended design. Patients in the PICU are scored with both PICU and non-PICU type sepsis scores and can trigger a non-PICU BPA. There is a mismatch between sepsis scores and sepsis BPAs within the ICU sepsis scoring tool. Additional questions include whether the mismatching of scores and BPAs has a significant impact on the tool’s overall performance. This calls for further investigation into the timing, performance and outcome metrics of the ICU sepsis scoring tool.