Public Health & Prevention
Public Health & Prevention 4
349 - Effectiveness of Nurse Home-Visiting for Birthing People with Previous Live Births
Publication Number: 349.448
- MA
Mandy A. Allison, MEd, MD, MSPH (she/her/hers)
Associate Professor of Pediatrics, Co-Director Prevention Research Center for Family and Child Health
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background:
Nurse-Family Partnership (NFP) is effective for first-time parents. The theoretical basis of NFP suggests that results may differ for people with previous live births (multips). Evidence for effectiveness among multips from other home-visiting programs is limited.
Objective:
Leverage a large, formative study of NFP for multips conducted 2017-2021 to estimate the program impacts of NFP for improving pregnancy, birth, and preventive care outcomes compared to matched Medicaid multip controls who did not receive NFP.
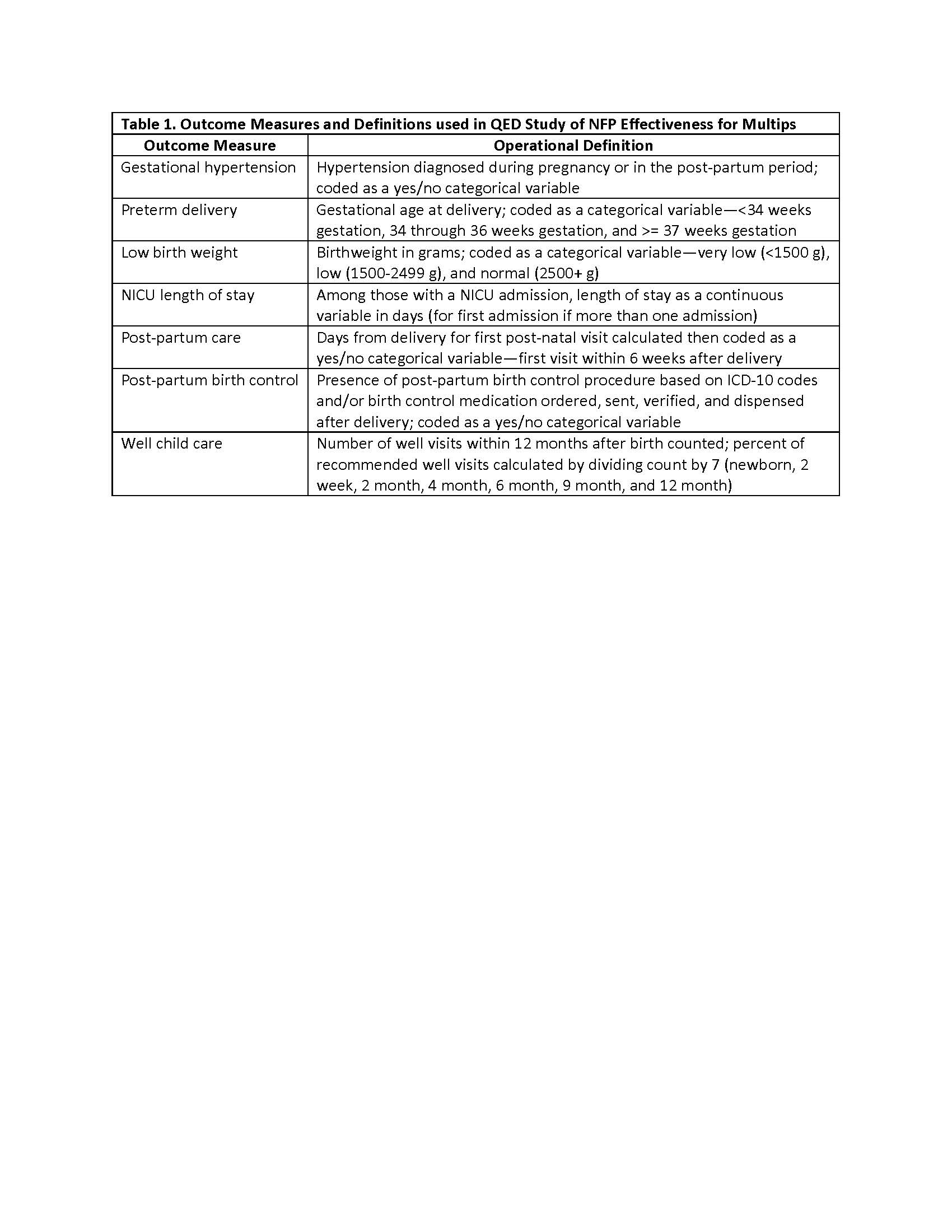
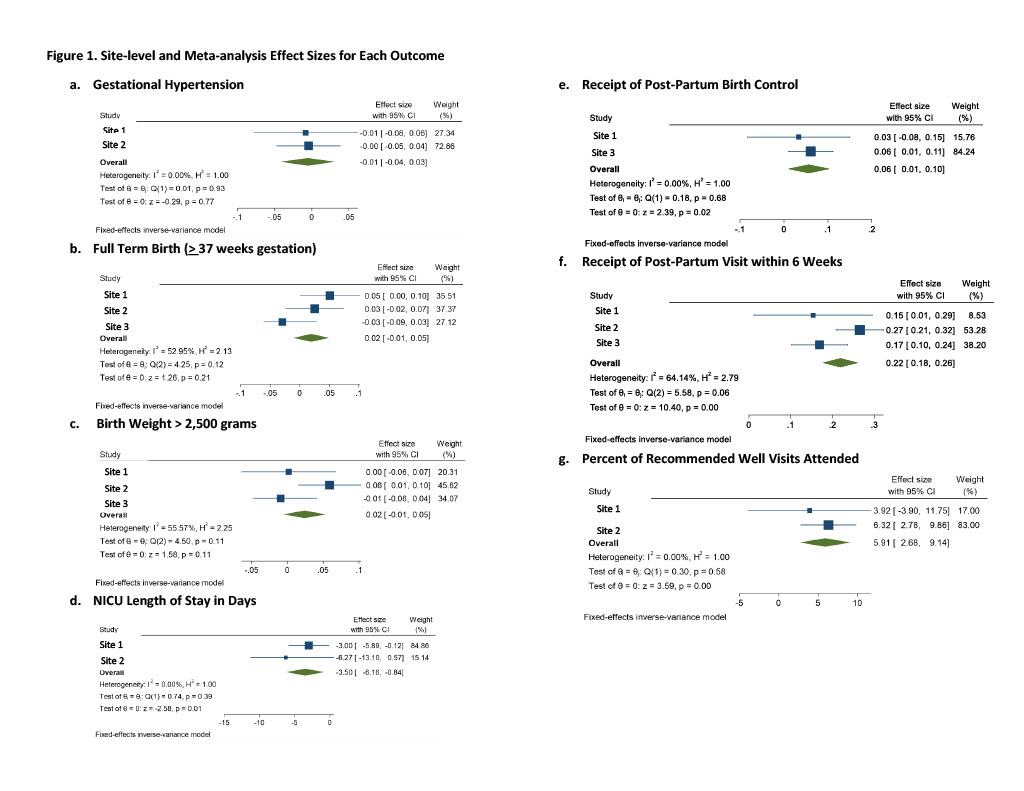
Design/Methods: We conducted a retrospective, quasi-experimental design study with NFP and Medicaid health plan partners serving multips as part of a formative study at 3 sites in Illinois, Indiana, and Ohio. We used electronic medical record data from participating health plans and Medicaid multip controls to estimate site specific program effects using logistic or linear regression after propensity score weighting or matching (depending on site) using an average treatment effect on the treated approach. Global estimates across sites were generated using a fixed-effects inverse variance weighted meta-analysis approach. Outcomes and definitions are shown in Table 1; not all outcomes were available for every site.
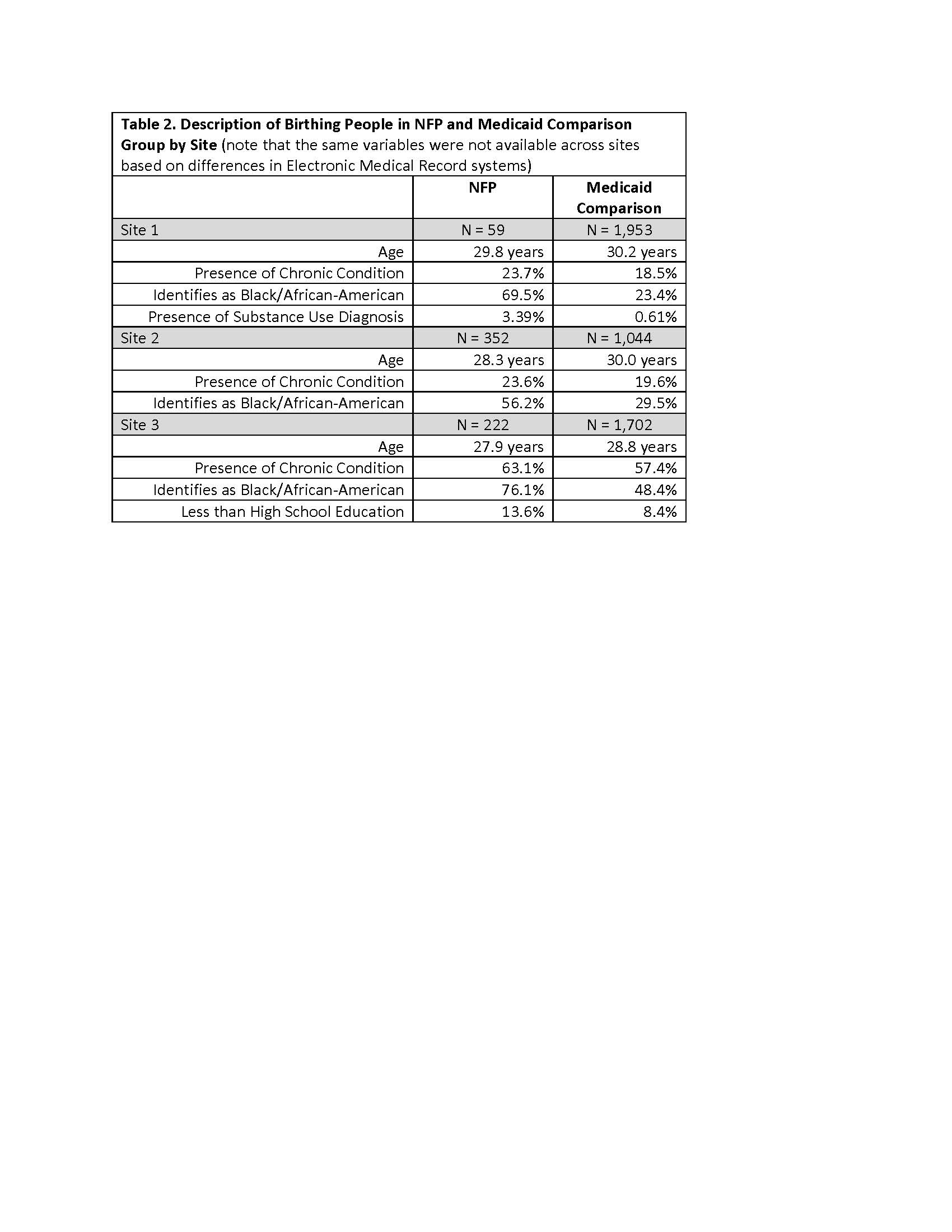
Results: NFP multips were at greater risk for poor health outcomes compared to Medicaid controls; Table 2 shows characteristics of NFP and comparison groups at each site (Site 1 NFP n=59, comparison n=1,953; Site 2 NFP n=352, comparison n=1,044; Site 3 NFP n=222, comparison n=1,702). No differences were seen for gestational hypertension, term birth, and birthweight (Figure 1). Positive effects for NFP multips were seen for receipt of post-partum birth control (coeff. 0.06, 95% confidence interval 0.01-0.10) and 6-week post-partum visit (0.22, 0.18-0.26), reduced NICU length-of-stay (-3.5, -6.16 to -0.84), and percent of recommended well child visits attended in first year (5.91, 2.68-9.14) (Figure 1).
Conclusion(s): NFP appears effective for reducing NICU length-of-stay and increasing receipt of preventive care among multips; however, selection bias may exist based on who elects to participate in NFP. We are now conducting a randomized clinical trial to minimize this bias and determine effectiveness of NFP for multips.