Infectious Diseases
Infectious Diseases 4
426 - Risk Factors for UTI Caused by ESBL-Producing Organisms in Children with Anomalies of the Urinary Tract
Publication Number: 426.418

Maria O. Valenzuela-Almada, MD (she/her/hers)
Pediatrics Resident
Childrens National - - Washington, DC
Washington, District of Columbia, United States
Presenting Author(s)
Background:
The global increase of multidrug resistant organisms (MDROs) and extended spectrum beta-lactamase (ESBL) producing organisms have led to an increase of urinary tract infections (UTIs) in children The presence of underlying congenital anomalies of the kidney and urinary tract (CAKUT) and neurogenic bladder (NGB) has been associated with both recurrent UTIs and increased risk of MDRO and ESBL-producing organisms.
Objective: To identify risk factors associated with UTI caused by ESBL-producing organisms in children with CAKUT/NGB.
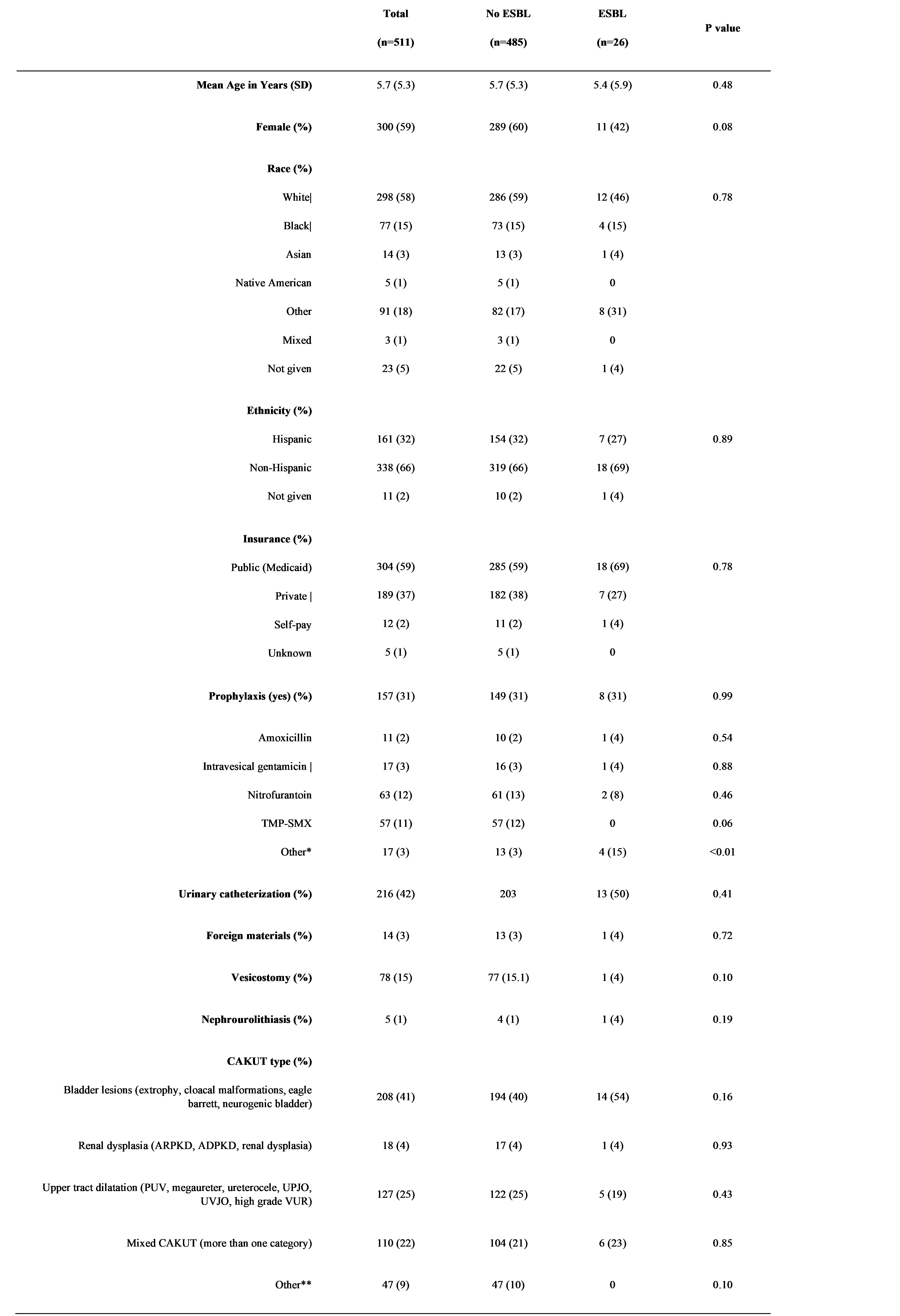
Design/Methods: This is a secondary analysis of data collected from a multicenter retrospective cohort study of children 0-17 years old with CAKUT/NGB who presented to the emergency department with fever or hypothermia and were diagnosed with UTI in 2017-2018. We excluded children with meningitis, end-stage renal disease, UTI within the past 30 days, surgical procedure within past 7 days, and renal abscesses. The outcome of interest was identification of an ESBL-producing organism in any of the urine cultures obtained, as defined per international consensus guidelines. Logistic regression identified factors associated with presence of ESBL-producing organisms.
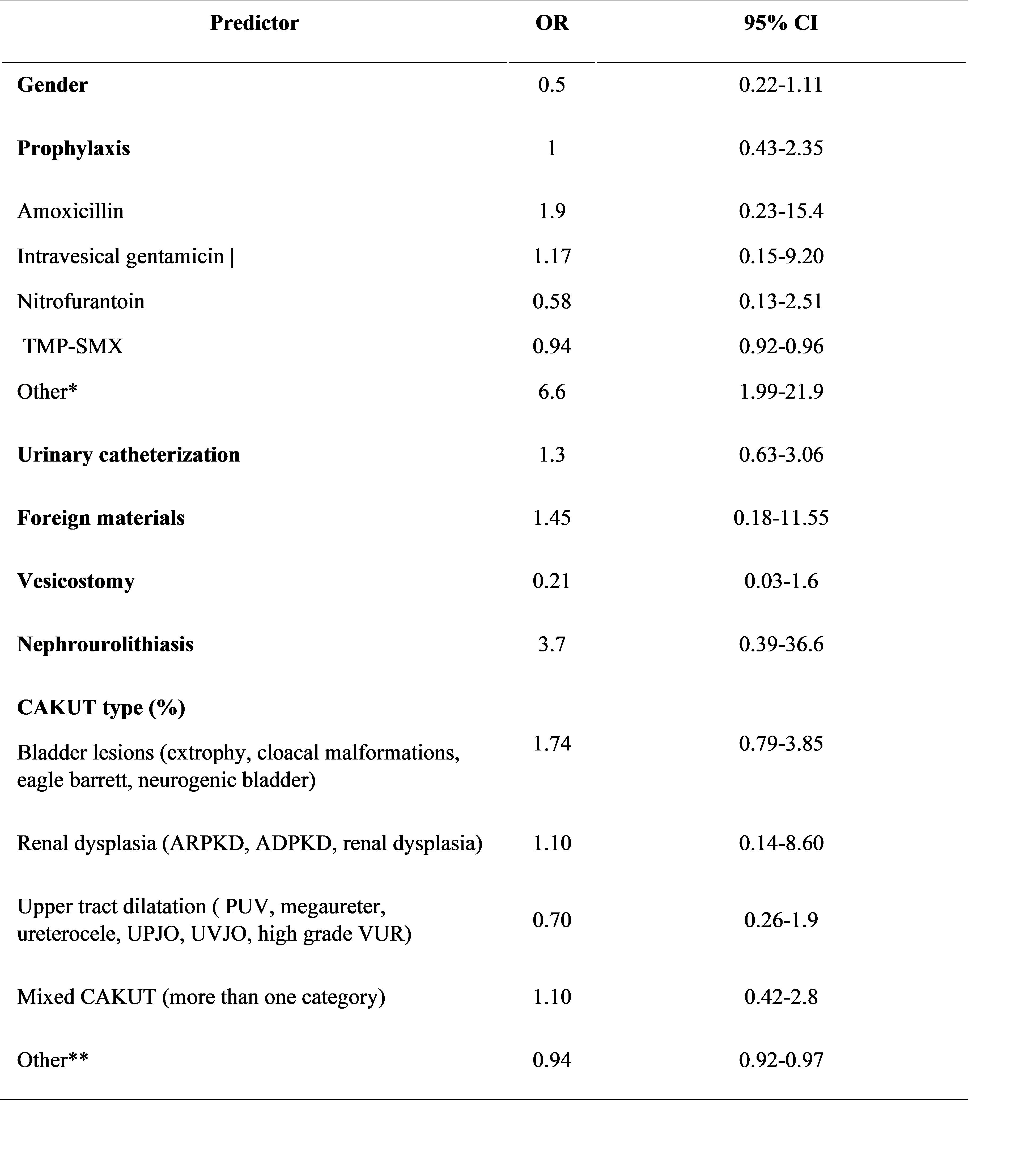
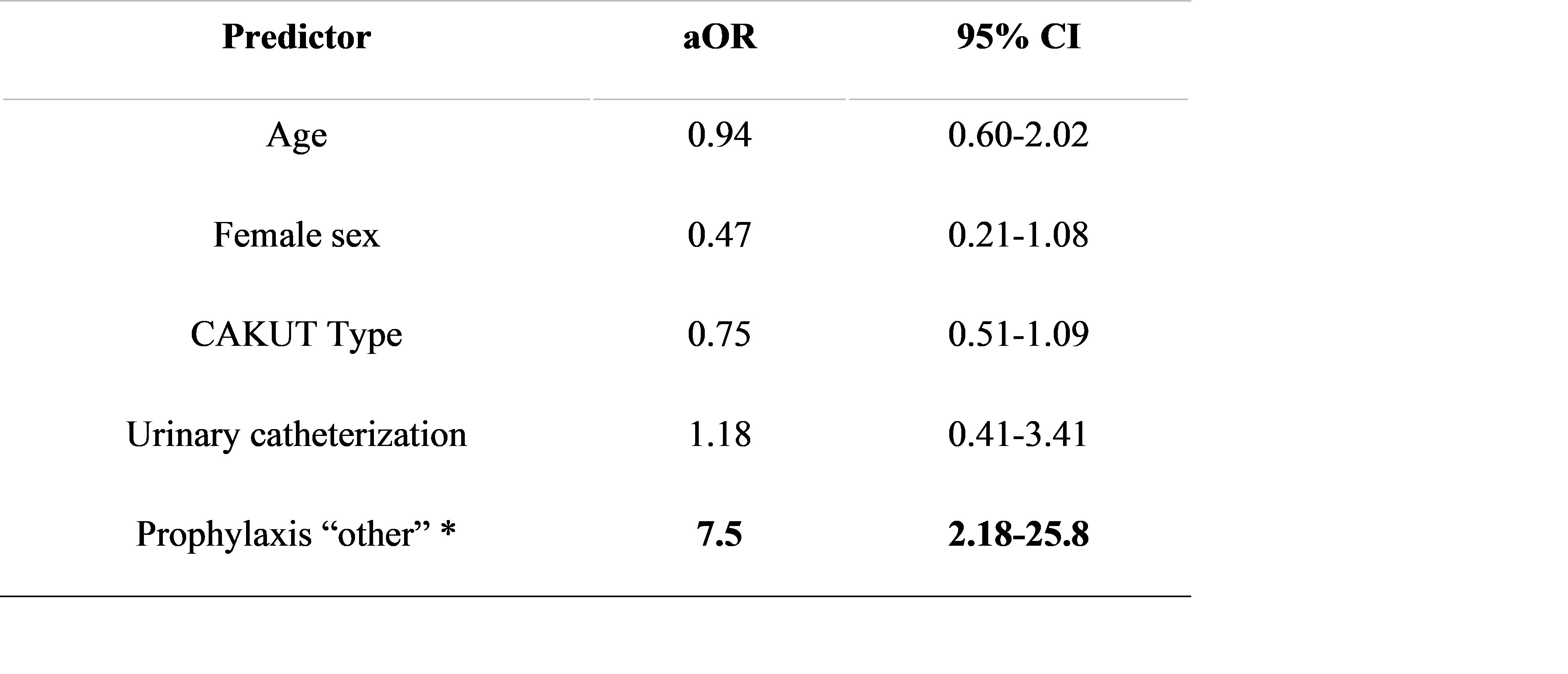
Results: 2032 patient encounters were identified, of which 511 were included. Fifty-two (10%) of the 511 included visits had an MDRO while 26 (5%) had an ESBL-producing organism identified. No difference was observed in the proportion of patients with ESBL UTI across CAKUT type. Presence of foreign materials, catheterization or use of antibiotic prophylaxis was not associated with ESBL UTI. When categorized by prophylaxis agent, use of non-standard agents (ciprofloxacin, intravesical amikacin cephalexin) for prophylaxis was associated with increased risk of ESBL UTI in both the univariate and multivariate analyses (OR 6.6, 95% CI 1.99-21.9; p< 0.01, aOR 7.5, 95% CI 2.18-25.8).
Conclusion(s): Contrary to findings in other studies, urinary catheterization, and presence of foreign materials were not associated with increased risk of ESBL UTI in children with CAKUT. Although antibiotic prophylaxis use generally was not associated with ESBL UTI, prophylaxis with less commonly used antibiotics was associated with increased risk of ESBL UTI. This association may be confounded by the indication to start broader spectrum antimicrobials in patients with previous history of resistant organisms, a practice that is not generally recommended. Larger studies are needed to further examine these and others risk factors.