Emergency Medicine: All Areas
Emergency Medicine 14
381 - Identification of children with anaphylaxis who may not require ED care: a 30-center retrospective cohort study
Publication Number: 381.405
.jpg)
Tim Dribin, MD (he/him/his)
Assistant Professor Emergency Medicine
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background:
National anaphylaxis guidelines recommend all patients treated with epinephrine in the community be transported to an emergency department (ED). However, this one size fits all practice recommendation has been questioned because reactions necessitating > 1 dose of epinephrine are rare.
Objective:
To identify children with anaphylaxis treated with epinephrine in the pre-ED setting for whom no further epinephrine was administered in the ED, potentially indicating that ED evaluation may not be necessary.
Design/Methods:
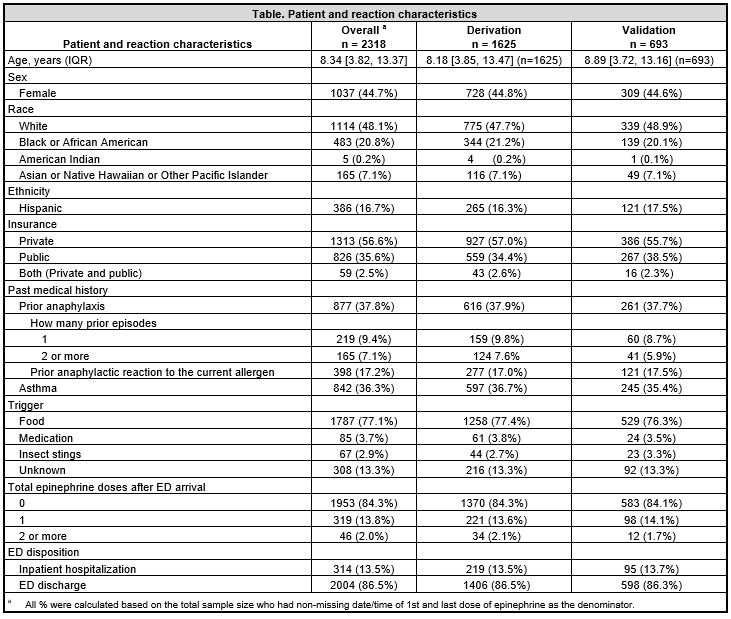
We conducted a retrospective cohort study across 30 North American EDs belonging to the Pediatric Emergency Medicine Collaborative Research Committee. Patients 6 months to < 18 years of age were eligible if they presented to a participating ED with anaphylaxis and received a single dose of epinephrine prior to ED arrival between October 2015 - December 2019. The primary outcome was receipt of epinephrine after ED arrival. Candidate predictors were limited to variables preceding ED arrival. We derived the rule in 70% of the cohort using LASSO regression and validated the rule in the remaining 30%. We sought to maximize the sensitivity and negative predictive value to minimize misclassifying patients as low risk who in fact received epinephrine after ED arrival.
Results:
2,318 eligible patients were included in the analyses. The median patient age was 8.3 years (IQR 3.8, 13.4), foods were the most common trigger (77.1%), and 365 (15.7%) patients received epinephrine after ED arrival (see Table). The rule included the following predictors of epinephrine administration after ED arrival: age > 10 years (OR 1.1 [1.0, 1.5]), history of anaphylaxis to current allergen (OR 1.2 [1.0, 1.5]), history of asthma (OR 1.3 [1.0, 1.6]), persistent symptoms after pre-ED epinephrine (OR 4.5 [2.8, 5.8]), pre-ED respiratory or cardiovascular involvement (OR, 1.1 [1.0, 3.5]), and no pre-ED antihistamine use (OR 1.0 [1.0, 1.4]). The prediction rule (absence of all risk factors) had a sensitivity of 97.3% and a negative predictive value of 91.8% for identifying patients that did not receive epinephrine after ED arrival.
Conclusion(s):
We derived and validated a clinical prediction rule to identify children with anaphylaxis who may not require ED care. Prospective refinement and validation of the rule and application in clinical care may reduce unnecessary ED utilization for anaphylaxis that can be safely managed in the community.