Infectious Diseases
Infectious Diseases 3
411 - Monthly Rates and Risk Factors for Invasive Streptococcus pneumoniae Infections in US Military Dependents before and during COVID-19
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 411
Publication Number: 411.417
Publication Number: 411.417
Matthew Penfold, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Fairfax, VA, United States; Sarah Prabhakar, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Silver Spring, MD, United States; Michael Rajnik, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, MOUNT AIRY, MD, United States; Apryl Susi, Henry M. Jackson Foundation at USUHS, GWU, Bethesda, MD, United States; Cade M. Nylund, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; ELIZABETH HISLE-GORMAN, Uniformed Services University, Bethesda, MD, United States; Matthew D. Eberly, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, New Braunfels, TX, United States

Matthew Penfold, DO (he/him/his)
Fellow
Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine
Fairfax, Virginia, United States
Presenting Author(s)
Background: Streptococcus pneumoniae causes significant disease in pediatric patients around the world. After COVID-19 was declared a pandemic, most countries implemented interventions to prevent the spread of SARS-COV-2. One consequence of these actions was a significant decrease in cases of invasive pneumococcal disease (IPD). As these strategies have become less stringent, increasing rates of IPD have surfaced. The Military Healthcare System (MHS) is uniquely positioned to study IPD rates in its pediatric patients who live around the world, but enjoy ready access to medical services.
Objective: Describe IPD rates and risk factors in the US Military dependent population before and during the COVID-19 pandemic.
Design/Methods: Inpatient data from the MHS was used to perform a repeated monthly cross-sectional study evaluating differences in Streptococcus pneumoniae rates and risk factors before and during the COVID-19 pandemic. Data was collected from March 2018 through February 2022 with the first two years considered pre-pandemic, and the following two years divided into Year 1 and Year 2. Inclusion criteria were children 0-59 months of age within the MHS diagnosed with IPD during the study period using ICD-10 codes. Monthly rates and rate ratios of IPD were calculated using adjusted and unadjusted Poisson regression with several demographic variables and time period at diagnosis.
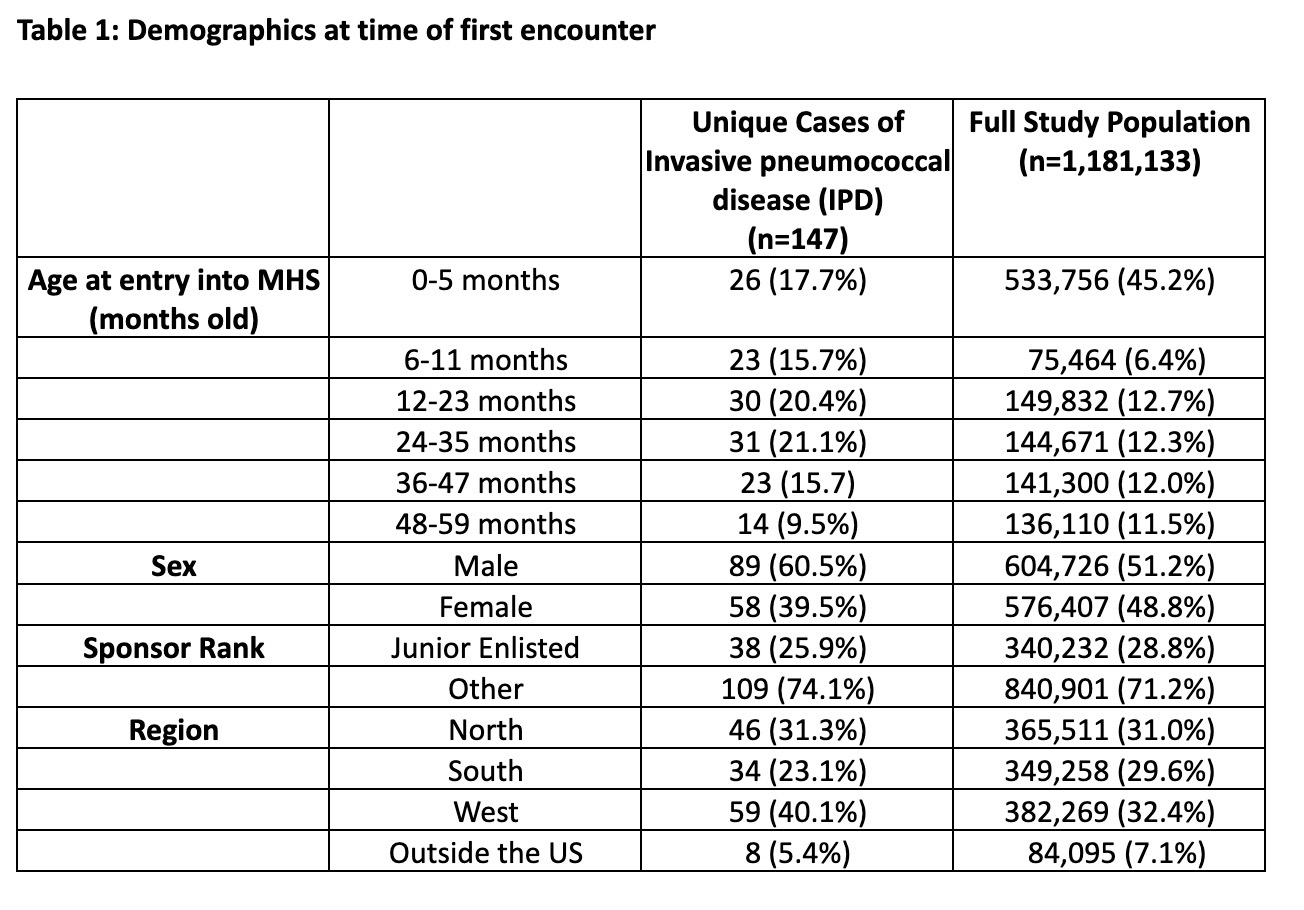
Results: Across the cohort of 1.1 million MHS beneficiaries, there were 147 unique cases of IPD in children less than 5 years old (Table 1). During the first year of COVID-19, there was a significant decrease in IPD cases compared to pre-pandemic. During the second year of COVID-19, rates of IPD returned to the pre-pandemic levels (Figure 1). For age, significant adjusted risk ratios were found in patients 0-5, 6-11, 12-23, and 24-35 months old, but not in 36-47 months old. Female sex was associated with decreased risk of IPD. Parent rank, as a marker of socioeconomic status, did not affect the risk of IPD. Lastly, patients living within the Tricare West Region, were found to have a higher risk of IPD (Table 2).
Conclusion(s): Within the MHS, there was a decrease in IPD rates during the first year of the COVID-19 pandemic, followed by a return baseline, both temporally associated with worldwide changes to strategies meant to reduce the spread of SARS-COV-2. Younger age was a risk factor for IPD, which is consistent with the well-documented epidemiology of Streptococcus pneumoniae infections.
.jpg)
.jpg)
