Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 9
577 - An Evaluation of Screening for Health Related Social Needs - Our FQHC Experience
Publication Number: 577.413

Margaret M. Tomcho, MD (she/her/hers)
Medical Director for Pre-Health Programs
Denver Health
Denver, Colorado, United States
Presenting Author(s)
Background:
Well-child visits (WCVs) are a cornerstone for optimizing not only child, but family health and wellness and are critical touchpoints for families that may not otherwise be routinely accessing healthcare. Identifying health-related social needs (HRSN) and facilitating resource connections are part of the essential community-clinical care continuum to optimize health and mitigate health disparities. Limited information exists on screening practices and how identification of needs varies among different populations.
Objective:
This evaluation examined implementation of the program at Denver Health’s (DH) Westside pediatrics, an urban Federally Qualified Health Center (FQHC) and identified lessons learned to inform expansion of screening and referral to other populations and health systems.
Design/Methods:
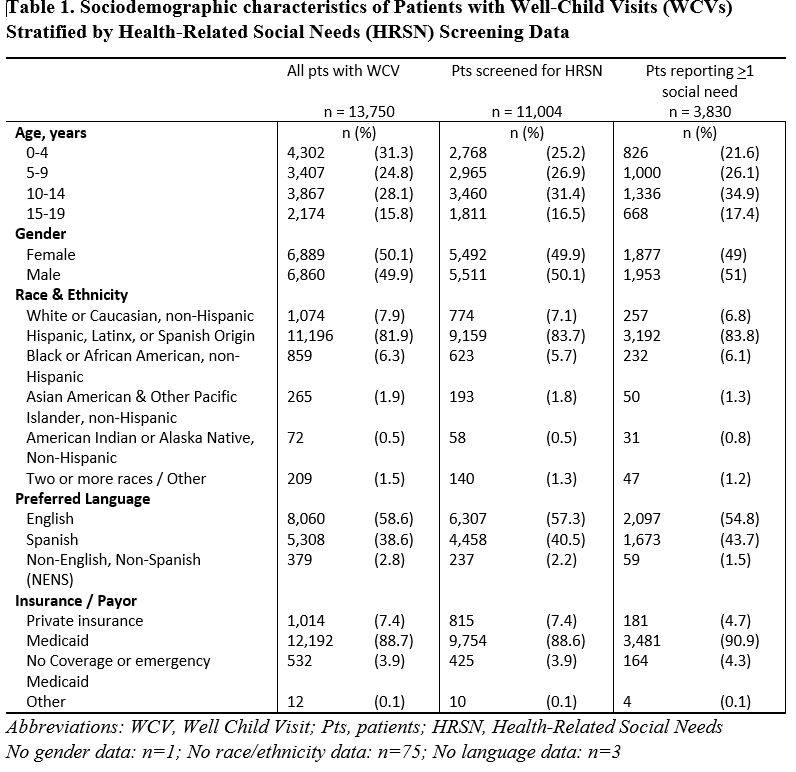
WCVs from June 1, 2020 through December 31, 2021 (N=13,750) were included. The Accountable Health Communities AHC HRSN screen was provided to caregivers at WCVs. Frequencies and proportions were used to describe patient characteristics of those that had a WCV, were screened, and who were identified with >1 social need. Multivariable logistic regression models with odds ratios (OR) and 95% confidence intervals (CI) were used to determine the association between patient characteristics and completing HRSN screening and having >1 social need.
Results:
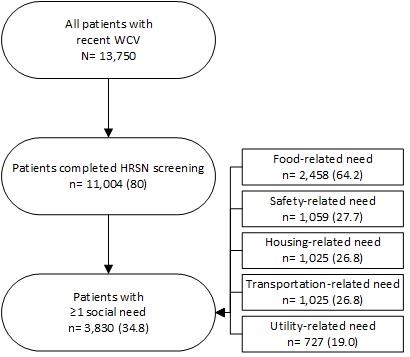
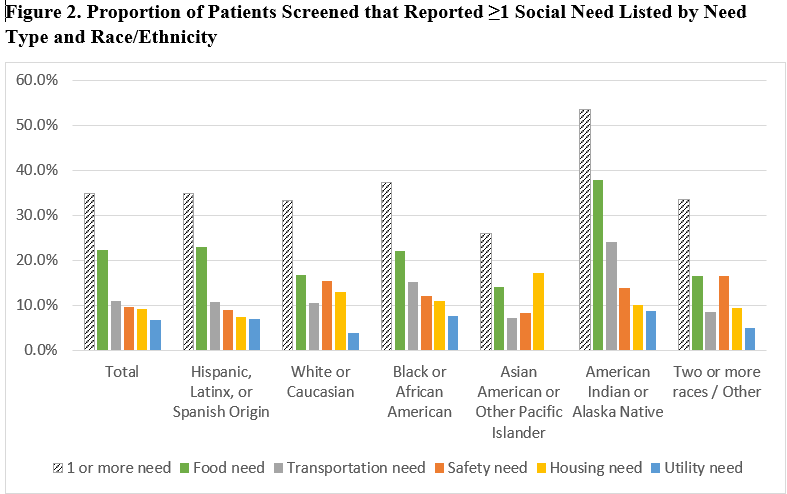
The tool was completed by 80% (n=11,004) of caregivers bringing children to a WCV at DH Westside pediatrics, with over one-third (34.8%; n=3,830) reporting >1 social need. Food insecurity was the most common concern (22.3%; n=2,458). Non-English, non-Spanish (NENS) speakers were less likely to be screened (OR 0.43, 95% CI 0.33, 0.57) and less likely to report a social need (OR 0.59, 95% CI 0.42, 0.82) than speakers of English, after adjusting for age, race/ethnicity, and health insurance.
Conclusion(s):
A high rate of screening indicates feasibility and acceptability of HRSN screening for pediatric patients in a busy FQHC. More than 1/3 reported one or more social needs, underscoring the importance to identity these needs and opportunity to offer personalized resources. Comparatively lower rates of screening and potential underreporting among NENS may be indicative of the availability and acceptability of current translation procedures and how the tool translates linguistically and culturally. Our experience highlights the need to partner with diverse community organizations and involve patients and families to ensure meaningful screening and personalized resource provision are part of culturally-appropriate patient-centered care.