Infectious Diseases
Infectious Diseases 1
623 - Risk factors associated with community acquired ESBL urinary tract infections in pediatric patients
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 623
Publication Number: 623.225
Publication Number: 623.225
Maria S. Rueda Altez, Children's National Health System, Washington, DC, United States; Yifeng Wang, The George Washington University, Washington, DC, United States; Maria C. Ortiz Vergara, Childrens national hospital, Gaithersburg, MD, United States; Rana F. Hamdy, Children's National Hospital, Washington, DC, United States; Anqing Zhang, George Washington University School of Medicine and Health Sciences, D.C., DC, United States; Anand Gourishankar, Children's National Health System, Washington, DC, United States

Maria Rueda Altez, MD (she/her/hers)
Clinical Fellow, Research Instructor
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background: Urinary tract infections (UTI) are one of the most common bacterial infections among infants and young children. Enterobacterales are isolated in more than 80% of pediatric UTI cases, and the rates of resistance are rising. Most pediatric studies focus on hospital-acquired resistant infections, but there has been an increase in community-acquired UTI cases caused by extended-spectrum beta-lactamase (ESBL) producing bacteria, for which risk factors are not clearly defined.
Objective: To determine the clinical and demographic risk factors associated with community-acquired ESBL UTIs in pediatric patients.
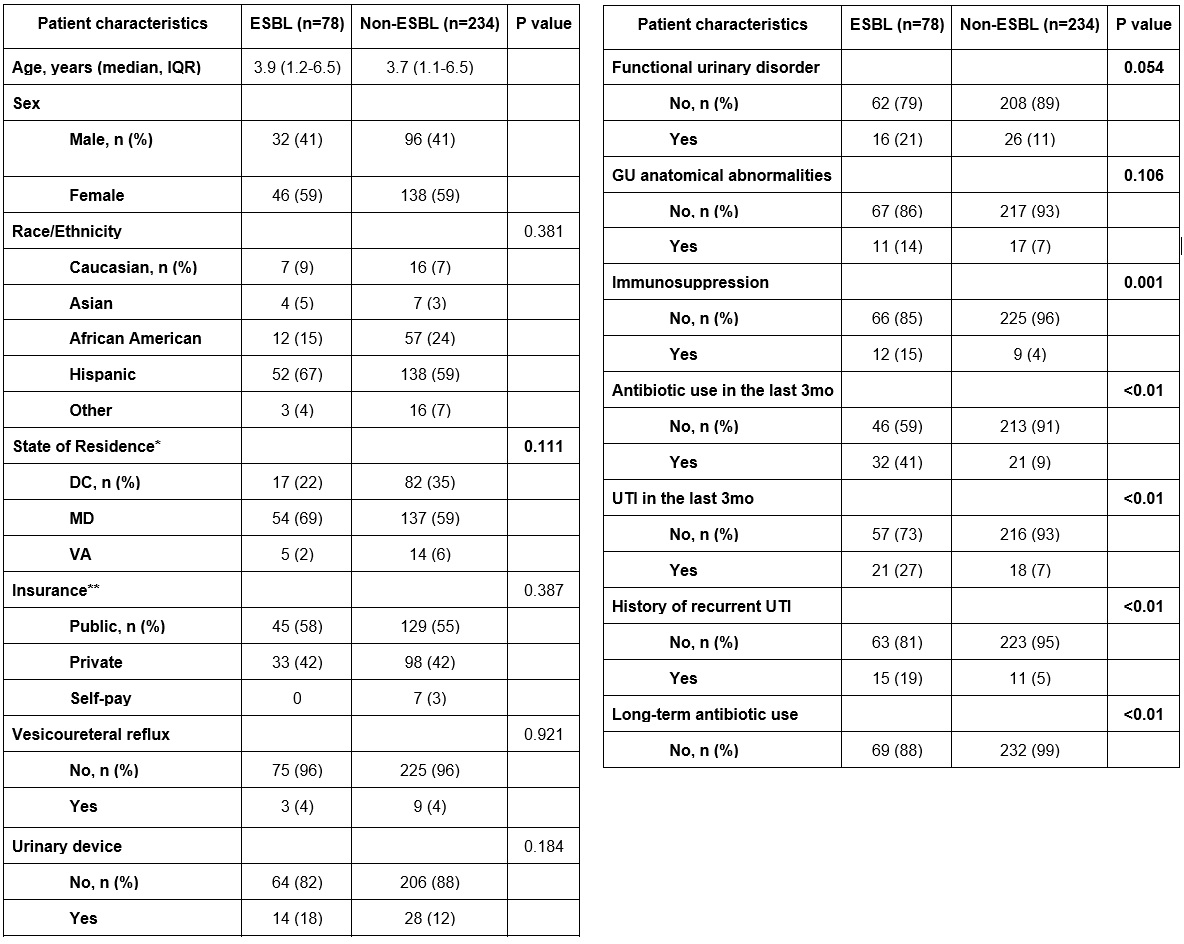
Design/Methods: We conducted a single-center retrospective case-control study at a tertiary teaching hospital. We reviewed urine culture information from January 2019 to December 2021 of patients evaluated in the emergency department. We identified those who met our study definition for community-acquired ESBL UTI: positive urine culture, abnormal urinalysis, symptoms consistent with UTI, and no hospitalization in the last 3 months. Only the most recent episode of UTI per patient was included. We randomly selected matched cases (ESBL UTI) to controls (non-ESBL UTI) by age and gender in a 1:3 ratio. We conducted a univariate analysis using Fisher’s exact test and developed a multivariate conditional logistic regression model to determine the association between each variable of interest and an ESBL UTI.
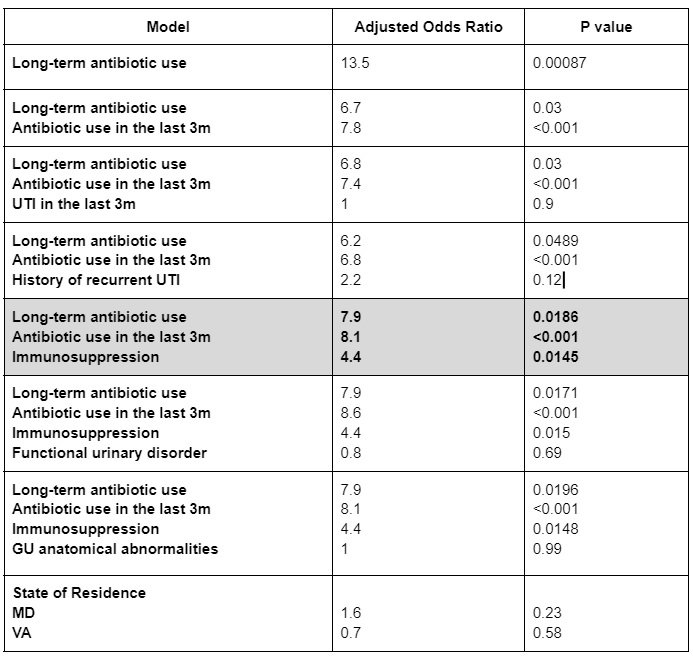
Results: A total of 312 patients: 78 cases and 234 controls were included. The median age was 3.8 years (IQR:1.2-6.5), and most patients were female (184, 59%) and Hispanic/Latino (190, 62%). The most common pathogen isolated was E. coli (82%). In the univariate analysis, state of residence, functional urinary disorder, genitourinary anatomical abnormalities, immunosuppression, antibiotic use 3 months prior to UTI, UTI in the last 3 months, history of recurrent UTI, and long-term antibiotic use approached significance (p< 0.15) and were included in the multivariate analysis. In the multivariate analysis, antibiotic use 3 months prior to UTI (OR 8.1, 95% CI 3.4-19.2), immunosuppression (OR 7.9, 1.4-44.4), and long-term antibiotic use (OR 4.4, 1.3-14.6) remained significant (p< 0.05).
Conclusion(s): Underlying immunosuppression, antibiotic use in the past 3 months, and long-term antibiotic use are independent risk factors for community-acquired ESBL UTI. Further research is needed to better identify patients at risk for resistant infections, optimize empiric management, and develop prevention strategies.