Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 6
764 - SHAREing is Caring: The Development of a Surgical Co-Management Program at Children's Hospital Colorado
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 764
Publication Number: 764.415
Publication Number: 764.415
Jason Zamkoff, Children's Hospital Colorado, Denver, CO, United States; Jessica Hedrick, Children's Hospital Colorado, Denver, CO, United States; Heather Bennett, Children's Hospital Colorado, Aurora, CO, United States; Justin Lockwood, University of Colorado School of Medicine, Aurora, CO, United States

Jason Zamkoff, MD
Pediatric Hospitalist
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
Background: Literature demonstrates that hospital medicine co-management of surgical patients can lead to decreased length of stay, decreased cost, decreased readmissions rates, and overall improved care. Review of a surge in serious patient safety events on Children Hospital Colorado’s (CHCO’s) medical-surgical floor revealed opportunities to improve post-operative care of hospitalized surgical patients. In response, we developed and implemented the Surgical Hospitalist Recovery (SHARe) Team.
Objective: The SHARe Team aims to: 1) provide individualized, comprehensive, optimal care to every co-managed patient it manages; 2) support medical-surgical nurses by providing quick responses, clear communication, and augmented education; and 3) make CHCO the nation’s flagship institution for surgical hospitalist co-management.
Design/Methods: Institutional leadership at CHCO funded 24/7 inpatient hospitalist coverage for SHARe Team. 10.4 clinical FTE was approved to support 2 APPs and 1 MD coverage during the day with MD Nocturnist coverage at night. A full day orientation process and hospitalist-surgical provider open-house was facilitated for all new SHARe Team providers, along with dissemination of a comprehensive educational handbook. Operational agreements were created with 13 surgical subspecialties. Patients designated for post-operative admission to this service included 1) those with highest medical complexity 2) those with prior operational agreements 3) those with no current inpatient surgical home/providers and 4) ad hoc admissions. Projected census was 22-24 patients per day on SHARe Team using these parameters. SHARe was implemented on 9/1/22. For preliminary evaluation we compared pre and post-SHARe implementation surgical inpatient hospital length of stay and emergency department return visits.
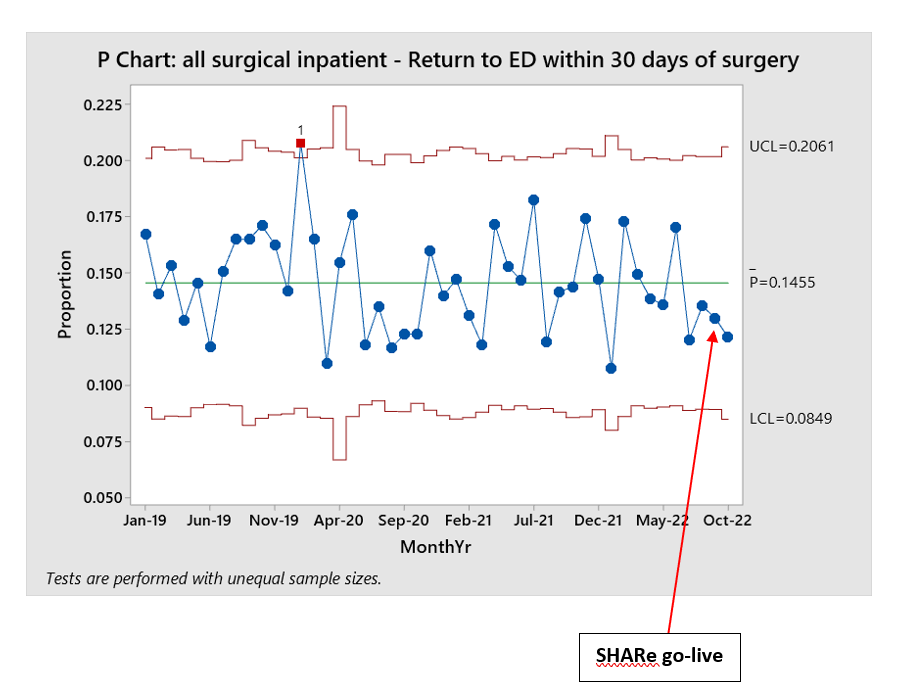
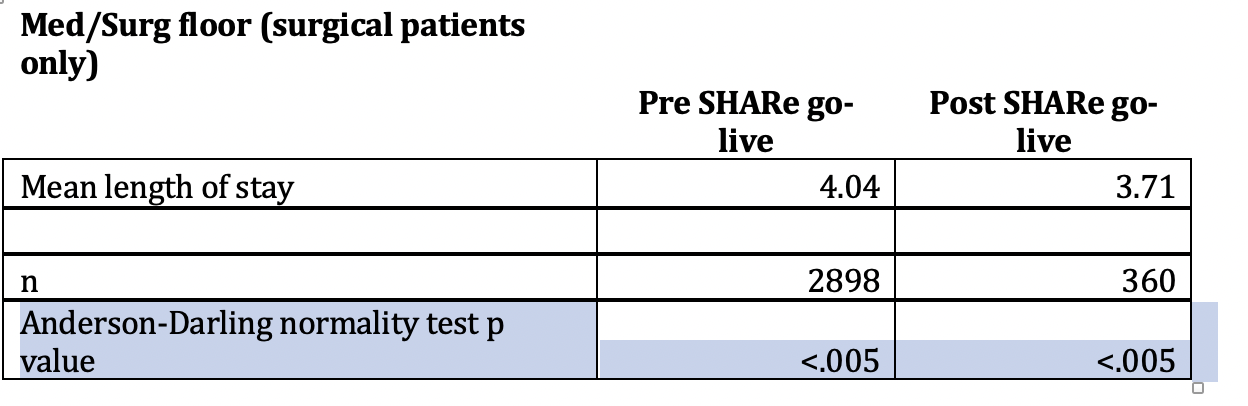
Results: Preliminary data (see charts below) demonstrates both decreased length of stay and decreased return to ED visits for ALL surgical patients on the medical-surgical floor at CHCO (not just SHARe Team patients). SHARe Team currently manages approximately 10% of all admitted surgical patients.
Conclusion(s): The SHARe Team at CHCO is a novel co-management service that may improve short-term outcomes amongst elective surgical patients admitted with the highest complexity and comorbidity. We believe the positive outcomes on SHARe Team are robust enough to demonstrate benefit for all surgical patients admitted. Further studies are needed to determine whether this team will sustainably reduce length of stay, readmissions and serious safety events. We also plan to assess patient, provider and nursing satisfaction.