Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 4
706 - Efficacy of Epinephrine Via Laryngeal Mask Airway in Neonatal Resuscitation in the Ovine Model of Asphyxial Cardiac Arrest
Publication Number: 706.445
- HA
Hamza F. Abbasi, MBBS (he/him/his)
Fellow physician
University at Buffalo
east amherst, New York, United States
Presenting Author(s)
Background:
Effective positive pressure ventilation (PPV) is the most crucial factor in the successful resuscitation of a depressed neonate, and often requires an advanced airway. Endotracheal tube (ETT) insertion is a highly skilled procedure that requires considerable training and experience. We have previously shown the laryngeal mask airway (LMA) to be as effective as the ETT PPV. The neonatal resuscitation program (NRP) recommends the first epinephrine dose to be administered via the ETT while establishing intravenous access via the umbilical vein. However, the efficacy of administration of epinephrine via the LMA has not been studied.
Objective: To compare the efficacy of epinephrine via the LMA to ETT during neonatal resuscitation.
Design/Methods:
This is a randomized controlled non-inferiority trial on a transitional asphyxiated near-term ovine model of complete cardiac arrest. Lambs were instrumented and resuscitated per NRP guidelines, then randomized to either LMA or ETT groups for PPV and epinephrine administration. A dose of airway epinephrine 0.1 mg/kg (1 ml/kg) was administered at 2 minutes of resuscitation. Subsequent epinephrine doses were administered via the umbilical venous line (UVC) at 5 minutes, then every 3 minutes until return of spontaneous circulation (ROSC) or 20 minutes of resuscitation. Hemodynamic parameters were continuously recorded. Blood sampling was done for blood gases and plasma epinephrine levels.
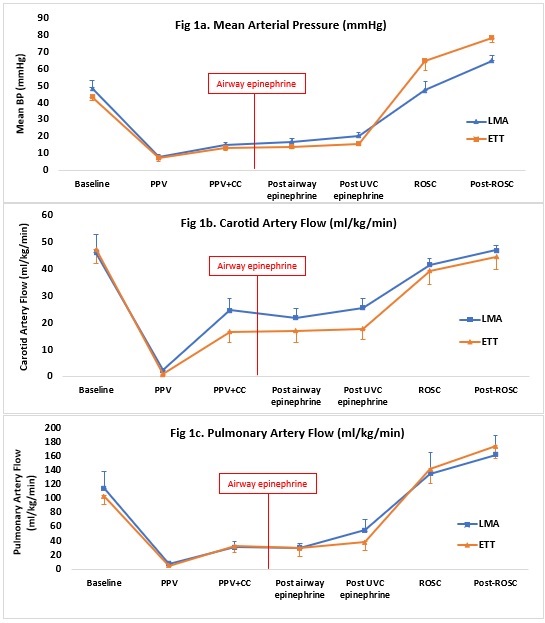
Results: 14 lambs were randomized, 8 in ETT group and 6 in LMA group. Baseline characteristics were similar between the two groups (Table 1). Incidence of ROSC was similar between the two groups (LMA 62.5% vs. ETT 66.7%; p=0.87). Time to ROSC was similar - 6.78 minutes +/- 58 seconds in the LMA group and 6.7 minutes +/- 65 seconds in the ETT group (p=0.92). Following airway epinephrine administration, mean blood pressures (p=0.27), carotid artery flow (p=0.47) and pulmonary artery flow (p=0.98) were similar between the two groups (Fig.1). There was no statistically significant difference in plasma epinephrine levels at baseline (LMA 0.7 +/- 0.5 ng/mL vs. ETT 0.8 +/- 0.2 ng/mL; p=0.88) and post-airway epinephrine administration (LMA 8.0 +/- 3.1 vs. ETT 7.8 +/- 4.6 ng/mL; p=0.85) (Fig. 2).
Conclusion(s):
There was no difference between ETT and LMA epinephrine administration during resuscitation on incidence/time to ROSC, hemodynamic parameters, or plasma epinephrine levels. The use of LMA epinephrine for neonatal resuscitation is a suitable alternative to ETT epinephrine..jpg)
.jpg)
