Neonatal General
Neonatal General 10: Outcomes
70 - Method of Home Tube-Feeding and Neurodevelopmental Outcome
Publication Number: 70.429

Tara L. DuPont, MD (she/her/hers)
Associate Professor
University of Utah
salt lake city, Utah, United States
Allison Fisher, MD (she/her/hers)
Fellow
University of Utah
Salt Lake CIty, Utah, United States
Presenting Author(s)
Co-Author(s)
Background:
Historically, stable infants, who have not achieved adequate oral intake, were discharged from the Neonatal Intensive Care Unit (NICU) with a surgically placed gastrostomy tube (GT). Evidence demonstrates the safety, cost-effectiveness, and practicality of discharge home with a nasogastric feeding tube (NG). In 2016, the Intermountain Hospital System adopted a home NG feeding program. There is an association between GT and neurodevelopmental impairment. It is unclear if infants discharged on home NG feeds also have neurodevelopmental impairment.
Objective:
To describe Bayley Scales of Infant and Toddler Development-III (Bayley-III) scores of infants discharged home with NG or GT feeding.
Design/Methods:
This was a retrospective study of infants seen at the Neonatal Follow-up Program through the University of Utah. Infants were included if they were born 05/2013 to 11/2020 and discharged with an NG or GT and had a Bayley-III at 2–3-years of age. Discharge feeding method was individualized through a shared decision-making model between the feeding team, clinicians, and family.
Results:
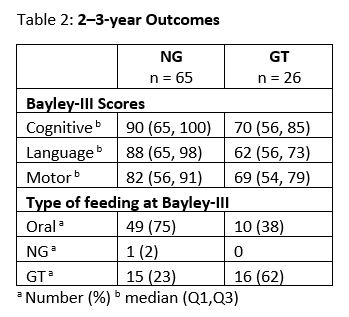
In Infants discharged with NG feeds 83% were extremely preterm with 35% having severe intraventricular hemorrhage (IVH) (Table 1). At follow-up, 75% of infants discharged with NG feeds achieved full oral feedings and 23% of infants had a GT placed (Table 2). Bayley-III scores were < 85 in: cognitive (42%), language (46%), and motor (54%). In Infants discharged with GT, 54% were extremely preterm and 12% had severe IVH. Bayley-III scores were < 85 in: cognitive (65%), language (88%), motor (81%). More than a third of infants discharged with a GT achieved full oral feeds at time of follow-up.
Conclusion(s): Infants discharged with NG tubes had cognitive and language scores in the low normal range. Most infants discharged home with NG feedings attained full oral feeding by 3 years. Infants with GT at NICU discharge had low Bayley-III scores at 2-3-year follow-up, consistent with previous studies. We did not identify a distinct patient demographic profile for infants discharged with NG or GT. Twice as many infants who were discharged on NG were receiving full oral feeds as those infants discharged with GT feeding. It was reassuring that preterm infants discharged with home NG feeding had Bayley-III scores within the normal range. We speculate that there are clinical factors related to placement of a GT that influence both neurodevelopmental outcome and attainment of oral feeding. .jpg)