Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 10
601 - Addressing Food Insecurity by Offering Utilization of a Clinic-Based Food Pantry
Publication Number: 601.411

Lilianna Suarez, MD, MPH
Medical Resident
Duke University
Duke University
Durham, North Carolina, United States
Presenting Author(s)
Background:
Many pediatric clinical practices are screening for food insecurity (FI) due to the known association with poor health outcomes. However, there is a known discrepancy between FI screening outcome and resource acceptance, with some patients screening negative for FI still interested in receiving food resources. Emerging evidence also suggests clinic-based food pantries may increase caregiver comfort discussing food needs and improve the likelihood of attending future clinic visits in addition to meeting a family’s food needs.
Objective:
To describe the overlap between FI screening outcome and clinic-based food pantry utilization and to evaluate changes in FI screening status after food pantry utilization.
Design/Methods:
From August 2020-July 2021, families presenting to a pediatric weight management program in Durham, NC were screened for FI using the Hunger Vital Sign. All were offered food from a clinic-based pantry irrespective of FI screening outcome. A chart review was conducted to collect sociodemographic and clinical characteristics. Multivariable logistic regression was used to explore changes in FI screening status after food pantry utilization.
Results:
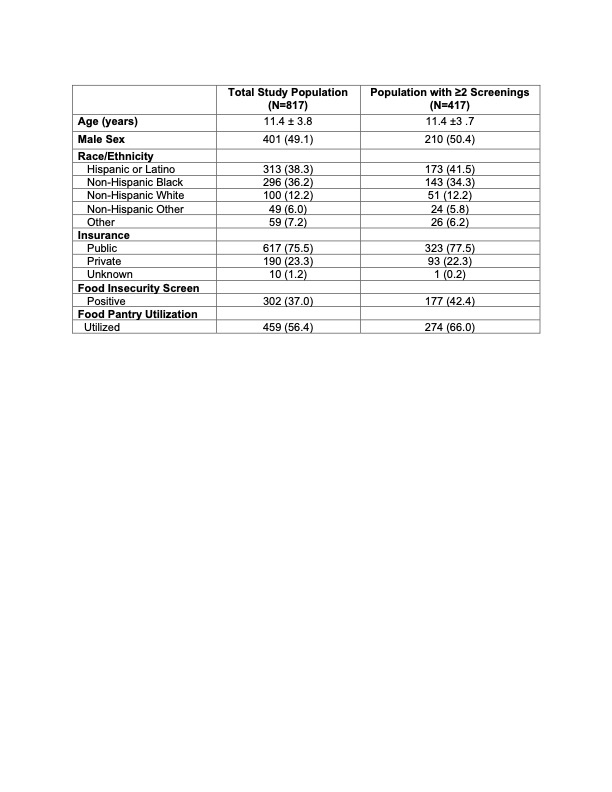
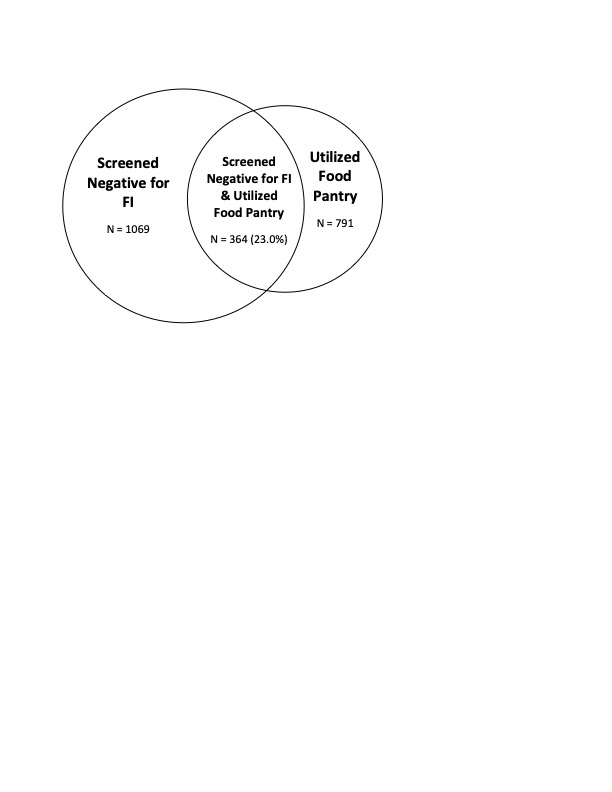
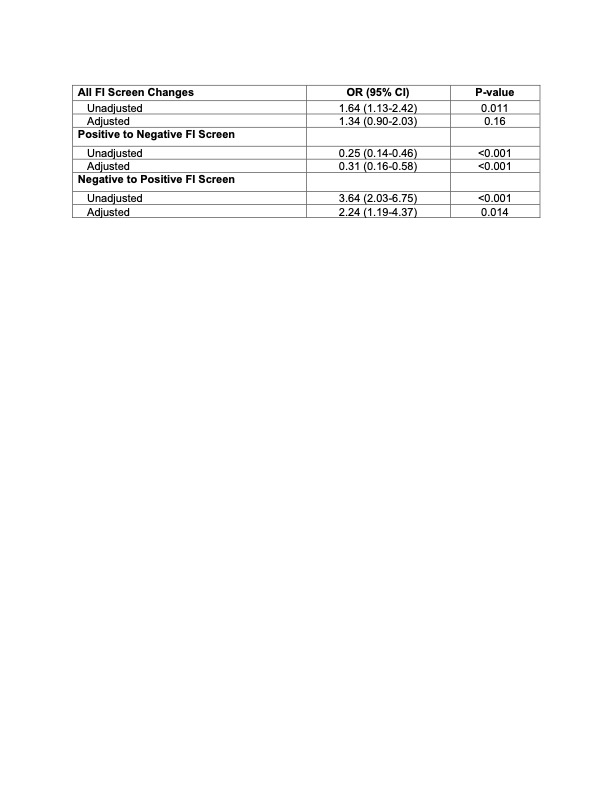
The cohort included 817 children and 1585 FI screenings, with 417 children screened at two or more clinic visits during the study period. Over a third (37.0%) of children screened positive for FI and over half (56.4%) utilized the food pantry (Table 1). Almost a quarter of screenings were families who screened negative for FI, yet utilized the food pantry (N=364, 23.0%; Figure 1). Positive FI screen and pantry utilization was associated with lower odds of negative FI screen at a subsequent visit compared to those with a positive FI screen who did not utilize the food pantry at a prior visit (OR: 0.31; 95% CI: 0.16-0.58; Table 2). Negative FI screen and utilization of the food pantry was associated with higher odds of positive FI screen at a subsequent visit compared to families with negative FI screen and who did not utilize the food pantry (OR 2.24; 95% CI: 1.19-4.37).
Conclusion(s):
Families screening negative for FI yet utilizing the food pantry were more likely to screen positive for FI at a subsequent visit, suggesting that utilization of a clinic-based food pantry may promote disclosure of true food needs. Universal offering of a clinic-based food pantry may also identify families who could still benefit from food assistance, but do not meet FI screening thresholds. Clinics should consider offering FI interventions at the time of screening to enhance identification of families with FI or those who may benefit from food resources.