Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 10
599 - Utilization of a Food Prescription Program for Patients with Food Insecurity and Elevated BMI
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 599
Publication Number: 599.411
Publication Number: 599.411
Suratha Elango, Baylor College of Medicine, Houston, TX, United States; Piyusha Kundu, Texas Children's Hospital, Houston, TX, United States; Patrice Morrow, Texas Children's Hospital, Houston, TX, United States; Anne Marie V.. Thompson, The Center for Children and Women - Southwest, Houston, TX, United States; Avni M. Bhalakia, Baylor College of Medicine, Houston, TX, United States

Avni M. Bhalakia, MD (she/her/hers)
Assistant Professor of Pediatrics
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Food insecurity and obesity often co-exist in patients as consequences of poverty. The lack of healthy and affordable food can make it difficult for families with food insecurity to maintain healthy weights. Food prescription programs that provide nutritious food are seen as a possible solution to addressing these health concerns.
Objective: We sought to measure the utilization of a food prescription program of enrolled patients, as well as determine if there was a change in patient BMI from those who utilized the program.
Design/Methods: We conducted a retrospective chart review of patients who were enrolled in a partner food prescription program between January 1, 2020 and December 31, 2021. The study was done at an urban clinic located in Houston, Texas, that serves patients with Medicaid or CHIP insurance only. Patients had to have an elevated BMI (>85%) and screen food insecure on the 2 question Hunger Vital Sign to be eligible for the program. The food insecurity screen was done at well check visits and relied upon clinic staff to identify a patient as eligible. Once enrolled, participants could access up to 30 pounds of produce and 4 healthy items from participating food pantries, twice a month. STATA was used for statistical analyses.
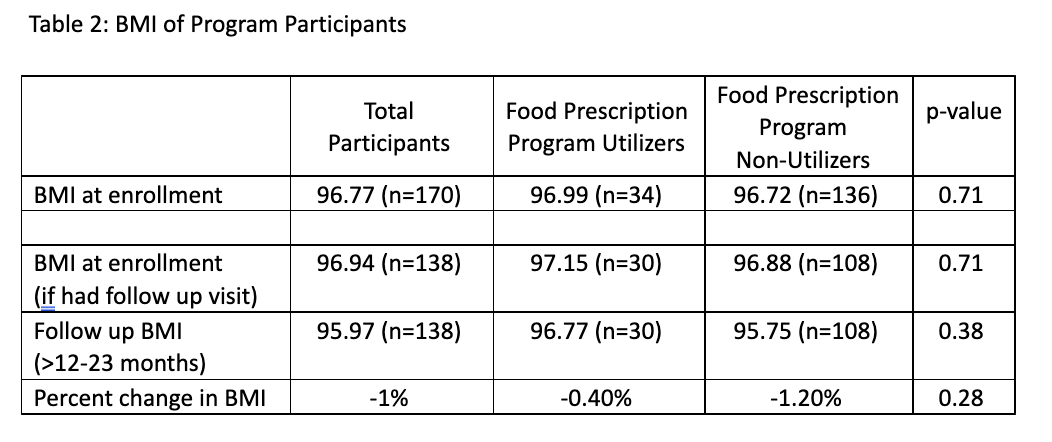
Results: Over the 24-month period, 170 patients, ages 2-18 years old, were enrolled into the food prescription program. Of the 170 patients, 64% were male, 70% Spanish-speaking, and 85% Hispanic. Demographics were similar between program utilizers and non-utilizers. Only 34 participants (20%) utilized the program and went to a food pantry at least once to receive food. Program utilizers visited participating food pantries an average of 5 times (range 1-23). The mean BMI of patients at enrollment was 96.77%. A one year follow up BMI was available for 138 enrolled patients (30 utilizers and 108 non-utilizers). The mean BMI for program utilizers decreased by 0.4% from 97.15% to 96.77%; the mean BMI for program non-utilizers decreased by 1.2% from 96.88% to 95.75%.
Conclusion(s): Of the patients who did utilize the food prescription program, there was not a significant change in BMI over the time period, which was one of the intentions of the food prescription program. A large majority (80%) of patients enrolled in the food prescription program did not utilize the program even once. Further investigation is needed to determine the barriers to utilization (e.g., transportation, pantry accessibility), as well as determine best methods to address child food insecurity and obesity from the medical home.
.png)