Global Neonatal & Children's Health
Global Neonatal & Children's Health 3
539 - Outcomes of Depression Treatment Among Pregnant Women with HIV in Uganda
Publication Number: 539.409

Laura J. Faherty, MD, MPH, MSHP (she/her/hers)
Physician Policy Researcher
RAND Corp. and Maine Medical Center
Cape Elizabeth, Maine, United States
Presenting Author(s)
Background:
Perinatal depression is common among women living with HIV and can adversely affect birth outcomes, maternal-infant attachment, and child development. While evidence-based treatments for perinatal depression exist, it is rarely diagnosed or treated in the Ugandan setting. Drawing on evidence-based collaborative care models for depression in low-resource settings, we are implementing a stepped-care approach to offering psychological and pharmacological treatment options for pregnant women living with HIV (PWLWH) in Uganda who meet criteria for depression.
Objective:
In this analysis, we examined (1) characteristics of women receiving Problem Solving Therapy (PST, a cognitive-behavioral intervention) versus antidepressant therapy (ADT), (2) treatment response by modality, and (3) correlates of treatment response.
Design/Methods:
We used data from 191 Ugandan women in the intervention arm of a cluster randomized controlled trial of task-shifted, stepped-care depression treatment for pregnant women living with HIV (PWLWH). Treatment response was defined as scoring < 5 on the nine-item Patient Health Questionnaire (PHQ-9). Bivariate analysis and multivariable logistic regression were used to examine patient characteristics in each treatment group and correlates of treatment response.
Results:
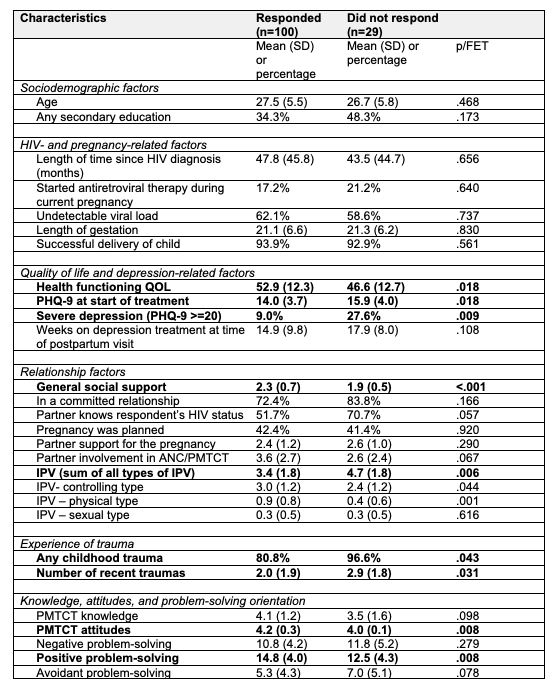
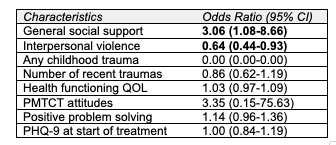
Nearly all (96%) participants meeting criteria for depression were treated: 84 received PST and 45 received ADT. Severe depression at treatment initiation was more common in those treated with ADT (28.9% versus 4.8%, Fischer’s Exact Test < 0.001) (Table 1). Treatment response was higher for PST (70/84; 83.3%) than ADT (30/45; 66.7%; p=.03). ADT side effects were rare and minor; no infants had serious congenital defects or required intervention for poor neonatal adaptation after in utero antidepressant exposure. Of 22 participants who did not respond to treatment, only four received intensified treatment per the stepped-care protocol. Social support and interpersonal violence were associated with treatment response in multivariate analysis (adjusted odds ratio, [aOR]=3.06, 95% CI=1.08-8.66 and aOR=0.64, 95% CI=0.44-0.93) (Table 2).
Conclusion(s):
Both depression treatment modalities yielded high response rates in Ugandan PWLWH, and ADT was well-tolerated by the mother-infant dyad. Our study is among the first to document the effectiveness of ADT in PWLWH in Uganda or the larger region of sub-Saharan Africa for alleviating perinatal depression. These results can help health care providers in low resource settings counsel their pregnant patients on the risks and benefits of depression treatment options.