Hypertension
Hypertension 2
29 - The Association of Socioeconomic Status and Preclinical and Clinical Cardiovascular Disease Risk Factors
Publication Number: 29.322
- SB
Sanjana Boyapalli, BA (she/her/hers)
Research Coordinator
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background:
Socioeconomic status (SES) is associated with hypertension and heart disease in adults. The association of SES with cardiovascular disease (CVD) risk factors such as blood pressure (BP), BP variability (BPV), and arterial stiffness in youth is less clear.
Objective: Determine the independent association of SES with BP, BPV, and arterial stiffness in youth.
Design/Methods: This was a secondary analysis of data obtained during two cross-sectional studies designed to assess the association of 1) diet and 2) mood with CVD risk factors. Participants underwent standardized anthropometric assessments, resting triplicate manual BP measurements, and 24-hr ambulatory blood pressure monitoring (ABPM). SES was defined using the Area Deprivation Index (ADI) which was determined by inputting home addresses into Neighborhood Atlas. Low/high SES was defined by median ADI value; low SES is indicated by high ADI (≥45), high SES is indicated by low ADI (< 45). BPV was determined by the standard deviation (SD) of wake ABPM measurements. The ambulatory arterial stiffness index (AASI) was calculated as (1- regression slope of diastolic on systolic ABPM values). Characteristics between youth with low and high SES were compared using t-tests, Wilcoxon rank sum, and chi-squared analyses as appropriate. Multivariable regression adjusting for age, sex, and obesity determined the association of ADI (continuous) and low SES (vs. high) with AASI, BPV, manual BP index (mean BP/age-sex-height specific 95th %ile BP).
Results: Seventy-eight children were included (mean age 15.1 yrs, SD=3.41; 56% Black; 51% female, 74% with obesity); 74 had AASI and 75 had BPV data available. A greater proportion of youth with low SES were male and Black race compared to youth with high SES. Those with low SES had greater adiposity, were more likely have second hand smoke exposure, and had greater systolic ABPM measurements. There were no differences in AASI or BPV between groups (Table 1). Low SES and ADI were each associated with systolic BPV in univariate and multivariable models adjusting for age and sex, however this association was no longer significant after further adjusting for obesity. ADI was similarly associated with manual SBP index, losing significance after additional adjustment for obesity (Table 2).
Conclusion(s):
Low SES is associated with CVD risk factors among youth, however these associations are likely explained by the increased prevalence of obesity in these youth. Obesity prevention and treatment remain effective strategies to decrease CVD. 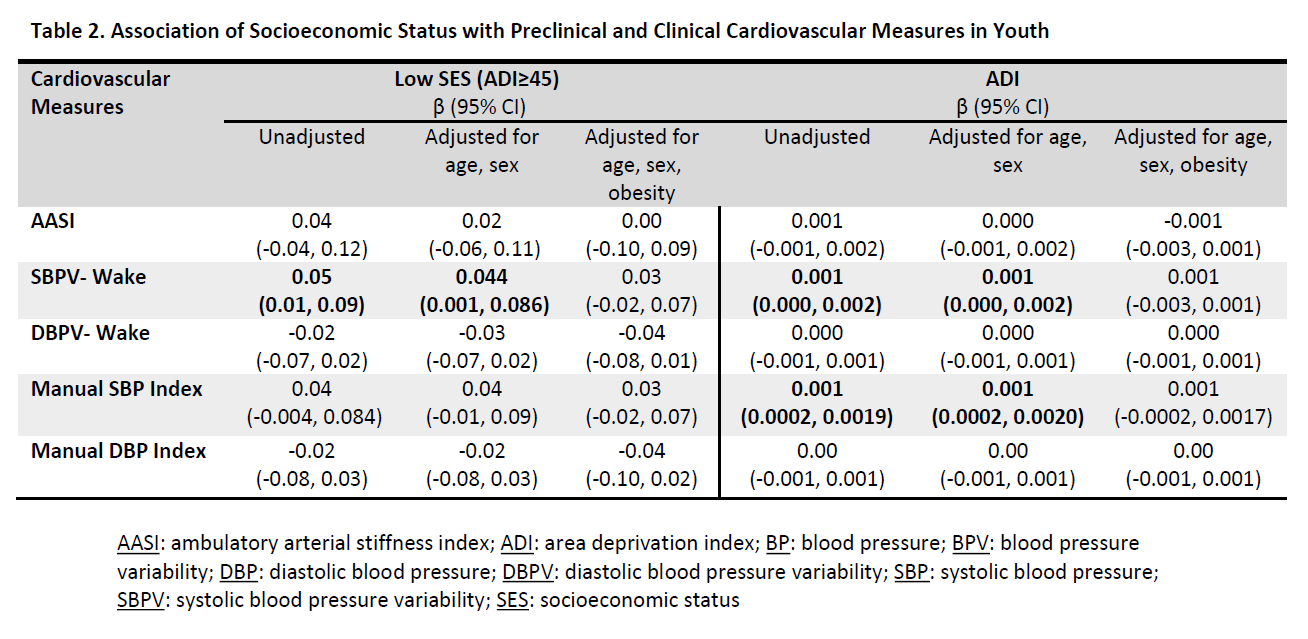
.png)
