Cardiology
Cardiology 2
759 - Prevalence of Dyslipidemia and Characteristics in Dyslipidemia Screening of Children with Congenital Heart Disease
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 759
Publication Number: 759.304
Publication Number: 759.304
Phillip S. Cheng, Nationwide Children's Hospital, Columbus, OH, United States; Jonathan A. Wheeler, Nationwide Children's Hospital, Columbus, OH, United States; Aaron Walsh, Nationwide Children's Hospital, Columbus, OH, United States; Kan N. Hor, Nationwide Children's Hospital, Columbus, OH, United States; Andrew H. Tran, Nationwide Children's Hospital, Columbus, OH, United States

Phillip S. Cheng, MD
Resident
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: Dyslipidemia is associated with increased risk for atherosclerosis and cardiovascular events in adulthood. However, the development of atherosclerosis begins in childhood with the universal lipid screening recommendations by the American Academy of Pediatrics (AAP) being an important part of identifying at-risk children. Children with congenital heart disease (CHD) are at higher cardiovascular risk but data are limited on the prevalence of dyslipidemia in this patient population.
Objective: We sought to determine the prevalence of dyslipidemia and different factors in lipid screening relative to patient characteristics in children with CHD.
Design/Methods: Children aged < 18 years with CHD who had primary cardiology encounters at Nationwide Children’s Hospital from 2003 to 2019 were included in the analysis. Anthropometric, demographic, lipid levels, and echo data were obtained if available. For those with lipid panels, subjects were classified as dyslipidemic (total cholesterol (TC) ≥ 200 mg/dL) or normolipidemic (TC < 200 mg/dL). Left ventricular mass indexed to height2.7 (LVMi-HT2.7) was calculated with left ventricular hypertrophy (LVH) defined as ≥ 38.6 g/ht2.7.
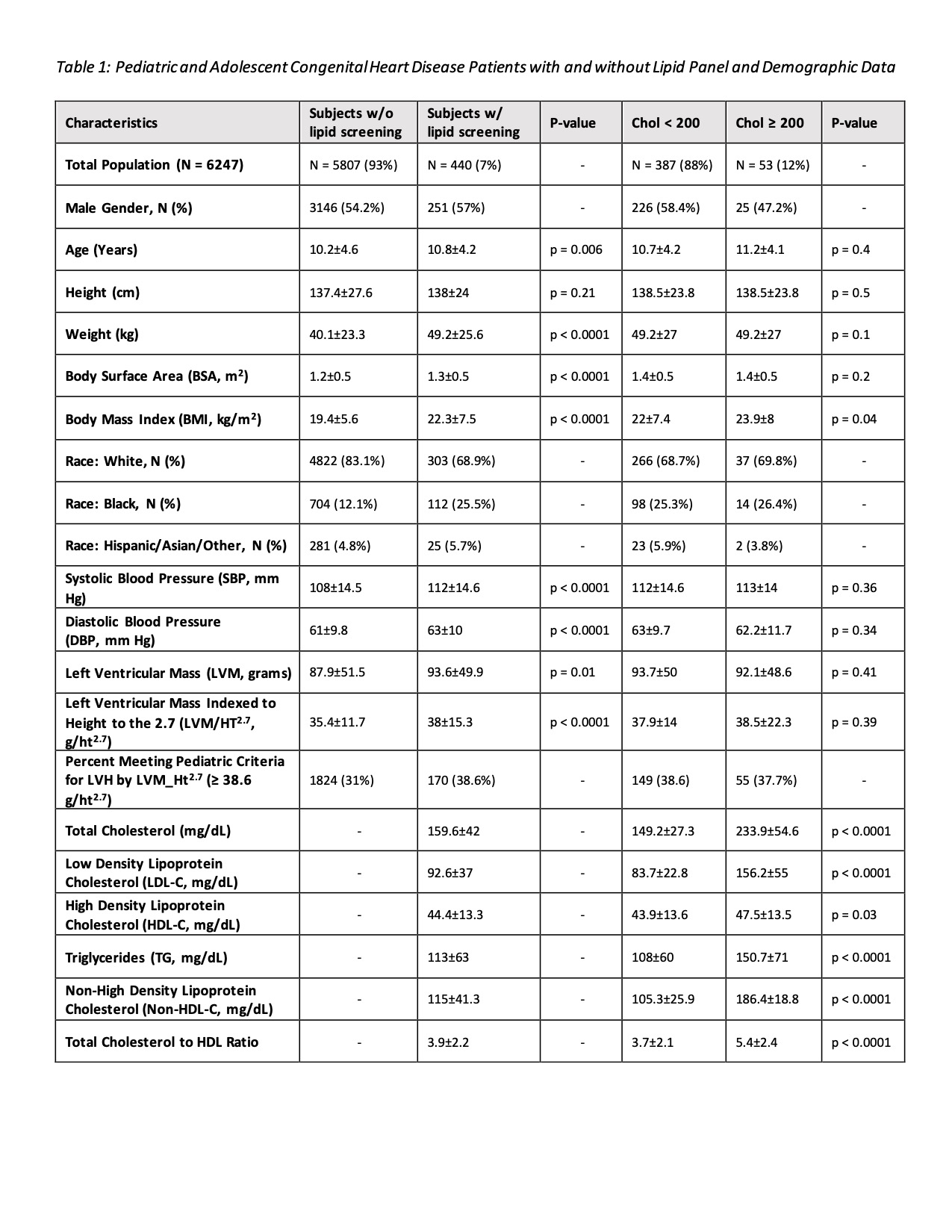
Results: Of the 6247 patients with CHD, we found that only 7% (N = 440/6247) were evaluated for dyslipidemia with findings detailed in Table 1. Of those screened, 12% (N = 53/440) had dyslipidemia. Screened subjects had higher mean BMI versus unscreened subjects (22.3 +/- 7.5 vs 19.4 +/- 5.6 kg/m2, P< 0.0001). Dyslipidemic subjects had higher mean BMI compared to those without (23.9 +/- 8 vs 22 +/- 7.4 kg/m2, P=0.04). Regarding race, of the total patient population 82% (N = 5125/6247) were White, 13% (N = 816/6247) were Black, and 4.9% (N = 306/6247) were Hispanic/Asian/Other. Black patients were screened at a high rate (13.7%, N = 112/816) compared to White patients (5.9%, N = 303/5125). Of Black patients screened, 12.5% (N = 14/112) were found to have dyslipidemia compared to 12.2% (N = 37/303) of White patients screened. We did not see differences in systolic blood pressure, diastolic blood pressure, LVM, or LVMi-HT2.7 in relation to those with and without dyslipidemia.
Conclusion(s): Only a small proportion of children with CHD had lipid screening performed despite AAP universal lipid screening guidelines. However, a sizable percentage of the children screened had dyslipidemia with similar rates of dyslipidemia between Black and White races. These findings emphasize the importance of screening for dyslipidemia in the at-risk population of children with CHD.