Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 2
227 - Early Screening Neonatal Echocardiography for Predicting Treatment of Patent Ductus Arteriosus
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 227
Publication Number: 227.33
Publication Number: 227.33
Jenny K. Koo, Sharp Mary Birch, San Diego, CA, United States; Katherine Coughlin, Neonatal Research Institute, Sharp Mary Birch Hospital for Women and Newborns, San Diego, CA, United States; Lydia Nashed, Inova Children's Hospital, Gaithersburg, MD, United States; Anup Katheria, Sharp Mary Birch Neoanatal Research Institute, University of California, San Diego School of Medicine, San Diego, CA, United States

Jenny K. Koo, MD (she/her/hers)
Neonatologist
Sharp Mary Birch
San Diego, California, United States
Presenting Author(s)
Background: Early screening neonatal echocardiography may predict morbidities and guide treatment in high-risk neonates. Preterm neonates are at high risk for developing a hemodynamically significant patent ductus arteriosus (PDA) resulting in hypotension, end organ injury, and intraventricular hemorrhage. While early treatment may reduce some of these morbidities, it also may result in overtreatment. Advanced measures may be challenging for most clinicians. Simple reliable measures of cardiac output may help clinicians decide which infants need early treatment.
Objective: To examine the association between echocardiographic markers obtained within the first 24 hours of life and need for treatment of a hemodynamically significant PDA.
Design/Methods: Patients with birth gestational age < 32 weeks from 2013 to 2022 had echocardiograms done within the first 24 hours of life as part of clinical trials and not used for guiding clinical management. Echocardiographic measurements include left ventricular output (LVO), right ventricular output (RVO), superior vena cava (SVC) flow, patent ductus arteriosus (PDA) diameter, and PDA direction of flow. Statistical analysis was performed on SPSS (v29). T-tests and chi-squared tests were done for continuous data and categorical outcomes, respectively. Logistic regression was performed to correct for gestational age. A receiver operating curve was created to optimize cut-off values.
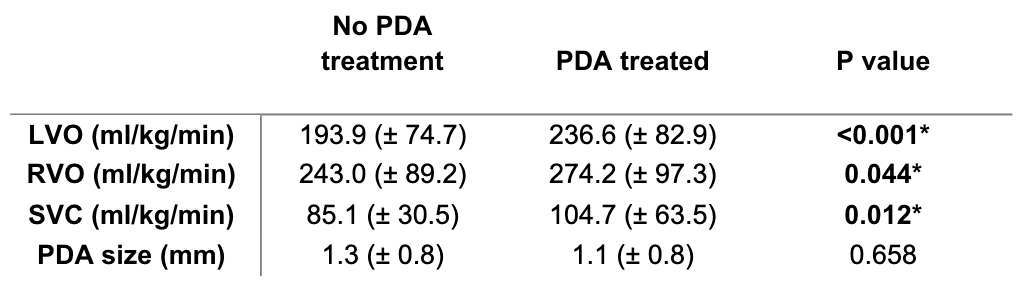
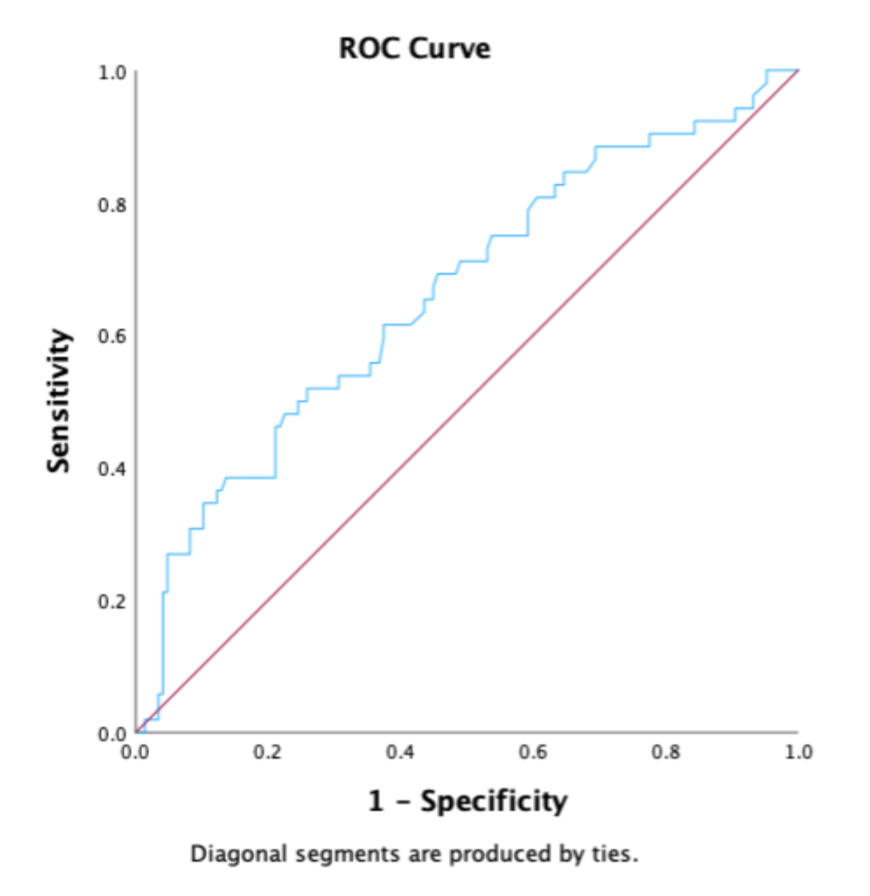
Results: 207 neonates were examined by early echocardiography. Infant characteristics are summarized in Table 1. There were differences in birth weight and gestational age in infants requiring PDA treatment. Patients who went on to require PDA treatment (pharmacologic or procedurally) had higher LVO (237 vs 194 ml/kg/min, p = 0.007), RVO (274 vs 243 ml/kg/min, p = 0.044) and SVC flow (105 vs 85 ml/kg/min, p = 0.012). PDA size did not differ between the two groups (Table 2). An LVO value greater than 204 ml/kg/min predicted a need for PDA treatment with a sensitivity of 63% and specificity of 66% (Figure 1).
Conclusion(s): Preterm neonates requiring PDA treatment exhibited higher markers of cardiac output (RVO, LVO and SVC flow). Although the sensitivity and specificity of an LVO greater than 204 ml/kg/day for predicting PDA treatment are only fair (63% and 66%, respectively), this echocardiographic marker has a strong negative predictive value of 81%. LVO alone may not be sufficient in defining a hemodynamically significant PDA. Further prospective studies will need to be performed to corroborate these associations between echocardiographic markers and clinical outcomes/morbidities.
.png)