Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 2: Physiology 1
336 - Influence of mechanical power on mortality and respiratory outcomes in very low birth weight infants intubated at birth
Publication Number: 336.345

Almudena Alonso-Ojembarrena, MD, PhD (she/her/hers)
Neonatologist
Puerta del Mar University Hospital
Cádiz, Andalucia, Spain
Presenting Author(s)
Background:
Recent research, mainly in adult settings with acute respiratory distress on invasive mechanical ventilation (IMV), relate the mechanical power (MP) with subsequent evolution.
Nowadays, there are no studies that assess the relationship of MP in preterm infants with long-term respiratory prognosis: our hypothesis was that preterm newborns who require intubation during the first day of life and receive greater MP, will have worse respiratory outcome or higher mortality.
Objective:
To compare the respiratory outcome and mortality in very low birth weight infants (VLBWI), who require intubation during the first day of life, based on the MP they receive. Likewise, we also intend to study the relationship between the lung ultrasound score (LUS) and the MP.
Design/Methods:
Prospective case-control study with VLBWI (birth weight less than 1500g at birth) born at our center, who required invasive mechanical ventilation on their first day of life. The study period was from January 2021 to April 2022.
Cases were VLBWI with invasive mechanical ventilation in the first 24 hours of life and either die before 36 weeks´ postmenstrual age (PMA) or develop bronchopulmonary dysplasia (BPD), in terms of requiring any respiratory support at 36 weeks’ PMA; controls were VLBWI intubated within the first 24 hours of life that survive until 36 weeks´ PMA, without BPD.
We recorded MP and LUS, in their first 24 hours of life, at the third, seven and fourteen days of life. MP was only calculated if the infant was still on IMV.
MP was calculated according to Formula 1, and indexed to the birth weight (J/min·kg):
Results:
We included 78 patients (27 were cases and 51 controls). Median gestational age (GA) was 27 weeks (interquartile rank (IQR) 25-29) in controls, and 26 weeks (IQR 24-28) in cases.
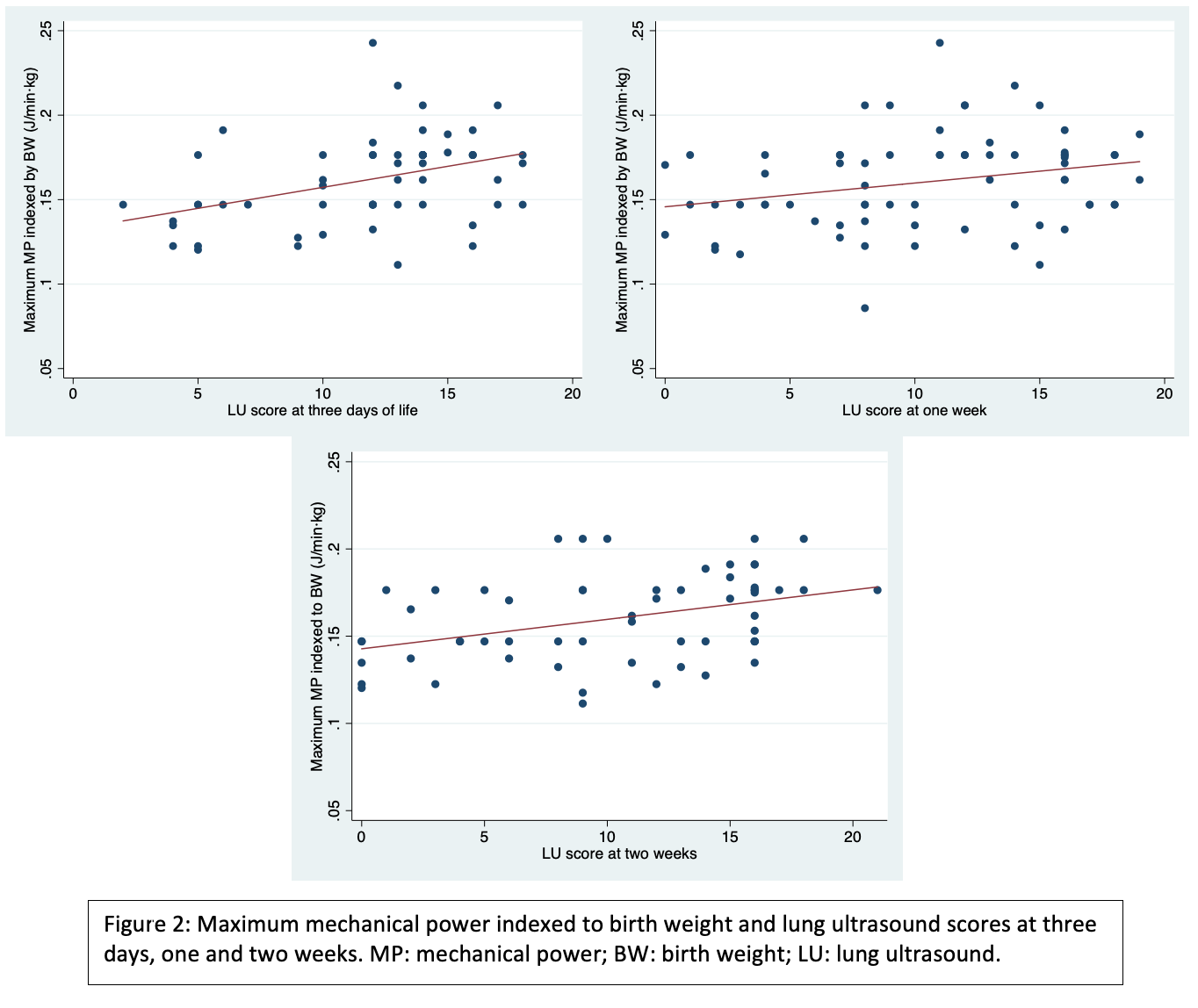
We found significant differences regarding the MP indexed by birth weight (MPBW) in the first 24h (controls: median 0.15 J/min·kg (IQR 0.14-0.16); cases: median 0.17 J/min·kg (IQR 0.15-0.18), p=0.02), and at the third day (controls: median 0.15 J/min·kg (IQR 0.13-0.17); cases: median 0.18 J/min·kg (IQR 0.15-0.18), p=0.04). There was a significant correlation between maximum MPBW and LUS at three days (Spearman rho=0.41, p=0.001)), at one week (Spearman rho=0.284, p=0.02)) and at two weeks (Spearman rho=0.4, p=0.001).
Conclusion(s):
VLWI with BPD or death before 36 weeks’ PMA received higher MPBW in their first 24 hours and at three days. Maximum MPBW during the first two weeks of life is correlated with LUS at three days, one and two weeks.
.png)
