Neonatal Quality Improvement
Neonatal Quality Improvement 3
732 - Standardizing Diagnosis of Urinary Tract Infections in the Neonatal ICU
Publication Number: 732.342
- BK
Benjamin C. Krasity, MD, PhD
Neonatal-Perinatal Medicine Fellow
Advocate Children's Hospital - Park Ridge
Park Ridge, Illinois, United States
Presenting Author(s)
Background:
Urinary tract infections (UTIs) are a common neonatal problem. When a culture obtained by bladder catheter is available, common diagnostic criteria include 50,000 or more CFU/mL of a single organism, or at least 10,000 CFU/mL with pyuria. Recently, evidence has emerged that a standardized approach can result in a reduction in the rate at which positive cultures are diagnosed as UTIs, without an increase in complications.
Objective:
The objective was maximizing the portion of diagnosed UTIs that conform to standard diagnostic criteria.
Design/Methods:
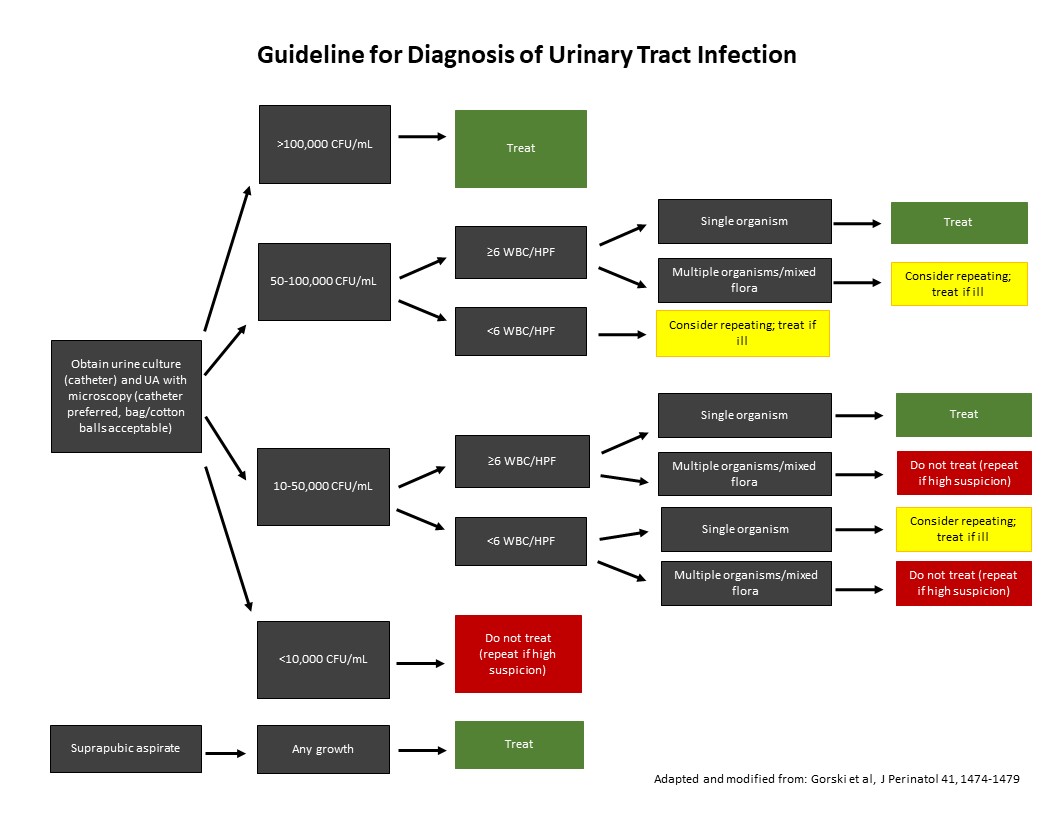
A UTI diagnosis guideline was adapted from the literature and modified with input from NICU and infectious disease specialists, then implemented in a level IV NICU. Urinalysis and urine culture results were assessed from 23 months prior to guideline implementation and 12 months afterwards. Periodic review was done to monitor adherence and for complications including subsequent UTI or urosepsis, necrotizing enterocolitis, renal scarring, hypertension, escalation of respiratory support, or death.
Results:
Guideline adherence after implementation was favorable. UA utilization increased significantly from 25.3% of cultures in the pre-intervention period to 91.6% afterwards. There was a non-significant increase in the portion of treated UTIs that conformed to diagnostic criteria, from 87% to 93%. There was also a modest and statistically insignificant decline in the portion of positive cultures diagnosed as UTIs, from 39% to 37%. There was no significant change in the rate of complications. In both periods, E. coli and Klebsiella species accounted for most treated UTIs, whereas Enterococcus faecalis was the most common organism judged to be a contaminant.
Conclusion(s):
The use of a guideline for approaching the diagnosis of UTIs can safely increase uniformity in practice. In contrast to previously published results, no significant changes were seen in the rate of UTI or the portion of diagnoses conforming to criteria for UTI. As the baseline rate of UTI diagnosis seen in our NICU was not particularly high, it is likely that guideline effects depend on the established practices of NICU providers. Additionally, a consistent pattern was seen in which organisms were more likely to be judged the source of true UTIs or contaminated cultures, meriting further study.