Neonatal General
Neonatal General 8: NICU Practices 2
186 - The Impact of Secondary Diagnosis on Neonatal Respiratory Extracorporeal Membrane Oxygenation Mortality and Complications
Publication Number: 186.332

Jotishna Sharma, MD, MEd (she/her/hers)
Director, Neonatal-Perinatal Medicine Fellowship Program
Children's Mercy Hospitals and Clinics
Kansas City, Missouri, United States
Presenting Author(s)
Background:
Extracorporeal membrane oxygenation (ECMO) is an established short-term cardiorespiratory strategy to support critically ill patients and traditionally has been offered to patients with a discrete, reversible disease. However, now neonates with highly complex additional diagnoses and diseases are being supported with ECMO. The impact of a secondary diagnosis on mortality and complications on neonates undergoing respiratory ECMO has yet to be evaluated. A greater understanding of this impact would help guide the medical decision-making.
Objective:
The objective of this study was to investigate the impact of secondary diagnoses on mortality and ECMO related complications of neonates undergoing respiratory ECMO.
Design/Methods:
This is a retrospective cohort study utilizing de-identified data of all neonatal patients undergoing respiratory ECMO between January 1st, 1992, and December 31st, 2021 (30 years), at Children’s Mercy Kansas City.
Results:
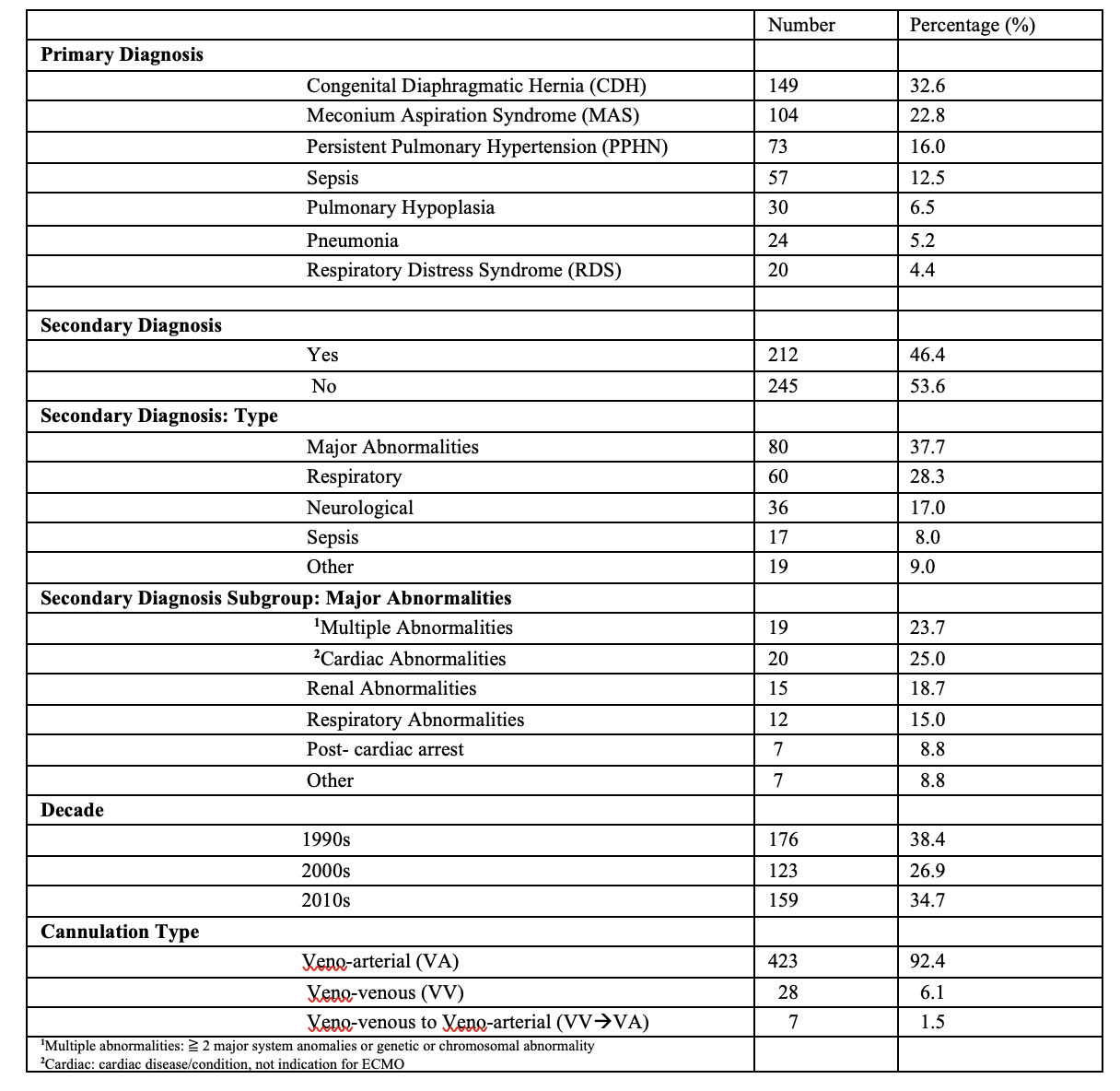
Total of 458 patients met the inclusion criteria. Two-thirds of the infants survived to discharge. The most common primary diagnosis was CDH (33%). 46% of patients had a secondary diagnosis, 1/3 of these patients had major abnormalities (Table 1). Primary diagnosis was significantly related to mortality (p< 0.0001) with pulmonary hypoplasia patients having the highest mortality (67%) and MAS having the lowest (7.7%). Secondary diagnoses were significantly (p< 0.0001) related to mortality with major abnormalities having the highest mortality (61%). The mortality was higher in the latter two decades (2000s and 2010s) (p= 0.0002). Lower gestational age, lower weight, longer ECMO duration, was significantly associated with mortality (p< 0.0001) (Table 2). 2/3 of patients had a minimum of one ECMO related complication with mechanical complications (37%) being the commonest. Those with a primary diagnosis of PPHN (p=0.0004), 2010s decade (p< 0.0001) and shorter duration on ECMO (p=0.0098) were significantly less likely to have complications. Complications were associated with primary diagnosis (CDH and sepsis), but not with having a secondary diagnosis (Table 3).
Conclusion(s):
As maternal, fetal, and neonatal care, advances rapidly in the 21st century, ECMO will remain a valuable tool. Patients that were previously excluded from receiving this type of support are currently being offered more frequently. Our study suggests patients with secondary diagnosis, especially those with major abnormalities may not benefit from ECMO. Further research with larger population size is needed to understand the survival and ethics of its use in these neonatal patients.
.png)
.png)
