Nephrology: CKD
Nephrology 5: CKD/ Diversity and Equity in Kidney Health
52 - Longitudinal Associations Between Collagen X Biomarker and Linear Growth Velocity In A Pediatric Chronic Kidney Disease Cohort
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 52
Publication Number: 52.35
Publication Number: 52.35
Denver D. Brown, Children's National Health System, Washington, DC, United States; Jennifer Roem, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States; Derek Ng, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States; RYAN COGHLAN, Shriners Hospitals for Children, Portland, OR, United States; Brian Johnstone, Oregon Health & Science University School of Medicine, Portland, OR, United States; William Horton, Molecular & Medical Genetics, Oregon Health & Science University / Shriners Hospital for Children, Ipswich, MA, United States; Susan L. Furth, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Brad A. Warady, Children's Mercy, Kansas City, MO, United States; Michal Melamed, Albert Einstein College of Medicine, Bronx, NY, United States; Andrew Dauber, Children's National Health System, Washington, DC, United States

Denver D. Brown, MD (she/her/hers)
Assistant Professor
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background: Collagen X Biomarker (CXM) is a byproduct of endochondral ossification that has been shown to be a biomarker of linear growth velocity.
Objective: We investigated whether CXM correlated with growth velocity (GV) in children with CKD.
Design/Methods: Our study used data from children 2-16 years old enrolled in the prospective Chronic Kidney Disease in Children (CKiD) cohort study. We assessed the association between CXM level and growth velocity based on height measurements obtained at study visits using linear regression models constructed separately by sex, with and without adjustment for CKD specific covariates. Linear mixed-effects models were used to capture the between-individual differences as well as the within-individual CXM changes over time associated with concomitant changes in growth velocity from baseline visit through follow-up.
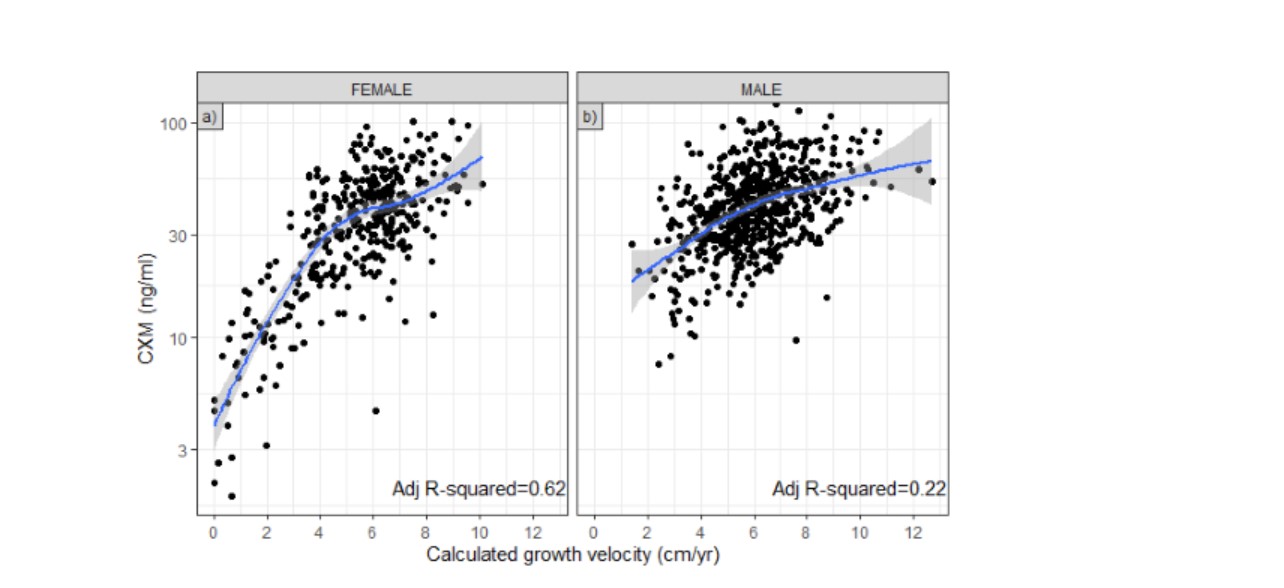
Results: A total of 976 serum samples from 213 participants were measured for CXM. CXM correlated more strongly in females compared to male participants (see figure). In models adjusted for CKD specific covariates, only severe proteinuria in female participants affected CXM levels. Finally, we quantified the between and the within participant associations between CXM level and a 1 cm/year change in growth velocity. A between participant increase of 25% and 15% in CXM level in females and males, respectively, correlated with a 1 cm/year higher growth velocity. Within an individual participant, a 28% and 13% increase in CXM values in females and males, respectively, correlated with a 1 cm/year change in measured growth.
Conclusion(s): CXM measurement is potentially a valuable aid in managing growth failure in children with CKD.