Neonatal Neurology: Clinical Research
Neonatal Neurology 5: Clinical
113 - Change in white matter injury volume and spatial distribution over time in very preterm infants.
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 113
Publication Number: 113.337
Publication Number: 113.337
Thiviya Selvanathan, The Hospital for Sick Children, Toronto, ON, Canada; Ting Guo, The Hospital for Sick Children, Toronto, ON, Canada; Vann Chau, The Hospital for Sick Children, Toronto, ON, Canada; Helen Branson, The Hospital for Sick Children, Toronto, ON, Canada; Anne Synnes, University of British Columbia Faculty of Medicine, Salt Spring Island, BC, Canada; Linh Ly, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Edmond N. Kelly, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Ruth E. Grunau, University of British Columbia, Vancouver, BC, Canada; Steven Paul. Miller, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada

Thiviya Selvanathan, MD (she/her/hers)
Pediatric Neurologist & PhD Candidate
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: White matter injury (WMI) is a common type of brain injury in very preterm infants. A decline in the prevalence of WMI in very preterm infants has been observed in one centre. However, it is unknown whether this decline has been seen across other centres and is associated with a change in the severity and spatial distribution of WMI.
Objective: To determine whether there has been a (1) decrease in WMI volume and (2) change in WMI spatial distribution over time across two prospective cohorts of infants born very preterm.
Design/Methods: 528 very preterm infants born < 32 weeks GA from two prospective cohorts across 3 NICUs were included in this study. Infants were categorized based on year of birth: epoch 1=2005-2009, epoch 2=2010-2014, and epoch 3=2015-2019. Infants underwent early-life (median 32.7 weeks post-menstrual age [PMA]) and/or term-equivalent-age MRI (median 41.3 weeks PMA). WMI severity was quantified as volumes. Non-parametric test for trends and multivariate linear regression model were used to assess WMI volumes across epochs of time. Probabilistic lesion maps were developed to assess the pattern of brain injury in infants across epoch of time.
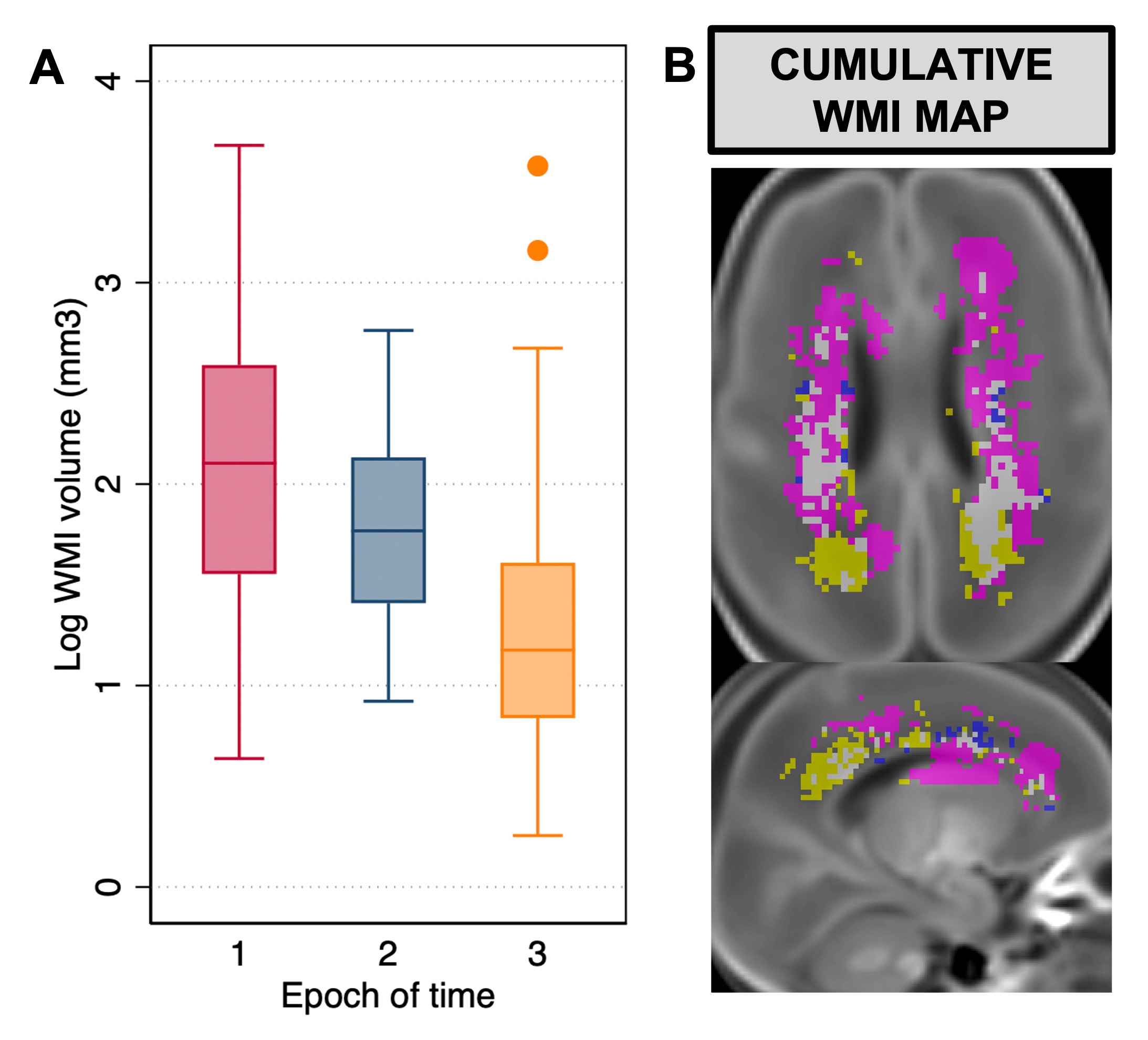
Results: WMI was seen in 152 (29%) infants. Infections (p< 0.001), retinopathy of prematurity (ROP; p=0.04), mechanical ventilation (p=0.05), and duration of indomethacin exposure were significantly different across epochs (p=0.01). WMI volume decreased over epochs of time (p< 0.001, Figure 1A). In a multivariable linear regression model, WMI volumes were smaller in epoch 3 compared to epoch 1 (b = -0.65, 95% CI [-0.91, -0.38], p< 0.001), even after adjusting for mechanical ventilation, infections, ROP, and indomethacin exposure. Duration of indomethacin exposure was an independent predictor of WMI volume in this model (b = -0.03, 95% CI [-0.07, -0.002], p=0.04). Probabilistic lesion maps revealed a shift from more central to posterior location of WMI across epoch of time (Figure 1B).
Conclusion(s): In this study, we observed a decrease in WMI severity, quantified as volume, over epochs of time, which persisted even after adjusting for important clinical confounders. We also found a change in the spatial distribution of WMI with a shift from more central to posterior predominant WMI over time. This finding may potentially reflect a decrease in white matter immaturity in very preterm infants across epoch of time. Further studies of associations of WMI with neurodevelopmental outcomes are warranted in contemporary cohorts of very preterm infants given this shift in WMI severity and location.
Funding: CIHR