Neonatal General
Neonatal General 9: NOWS and Other Exposures
203 - Risk Factors and Neonatal Morbidities Associated with Exposure to Maternal Substance Use in Preterm Infants Less Than 30 Weeks Gestational Age
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 203
Publication Number: 203.333
Publication Number: 203.333
Megan Chang, LAC+USC/USC Keck School of Medicine, Los Angeles, CA, United States; Rangasamy Ramanathan, Keck School of Medicine of USC, Los Angeles, CA, United States; Rowena Cayabyab, University of Southern California/LAC+USC Medical Center, Los Angeles, CA, United States

Megan Chang, MD (she/her/hers)
Neonatology Fellow
LAC+USC/USC Keck School of Medicine
Los Angeles, California, United States
Presenting Author(s)
Background: Maternal drug use during pregnancy is associated with adverse neonatal outcomes. Less is known about the effects of in-utero drug exposure among early preterm neonates.
Objective: Our study objective was to identify risk factors and neonatal morbidities associated with exposure to maternal substance use in preterm infants less than 30 weeks gestational age.
Design/Methods: Retrospective review of preterm infants less than 30 weeks gestational age (GA) admitted to a Level III neonatal intensive care unit (NICU) between 1/2017–10/2022. Maternal substance use of amphetamines, cocaine, opiates, cannabinoids, and benzodiazepines was determined by self-report and/or positive maternal or neonatal urine toxicology screens on admission. Maternal and neonatal data was collected from NICU database and electronic medical records to compare maternal and neonatal demographics and clinical outcomes of infants exposed and not exposed to maternal substance use.
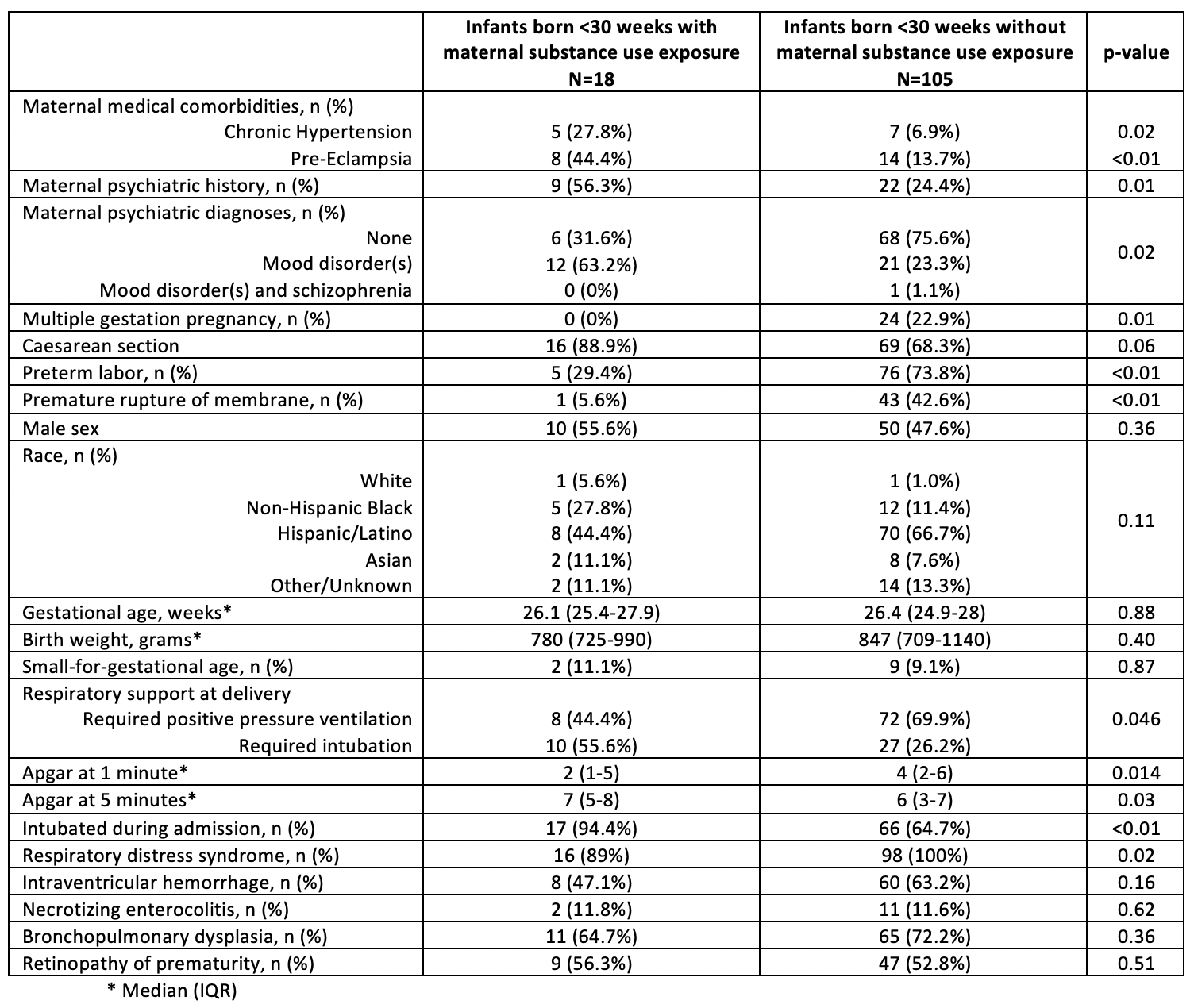
Results: There were 123 preterm neonates born less than 30 weeks’ gestational age identified, with 18/123 (15%) exposed to maternal substance use. Mothers with substance use had higher rates of medical and psychiatric comorbidities, including chronic hypertension, pre-eclampsia, and mood disorders. Mothers without substance use exposure had increased rates of multiple gestation, preterm labor, and premature rupture of membranes. There were no significant differences in neonatal demographics between the two groups, however, neonates with maternal substance exposure were more likely to have lower Apgar scores at 1 and 5 minutes and require intubation at birth. There were no significant differences in the rates of intraventricular hemorrhage, necrotizing enterocolitis, retinopathy of prematurity, bronchopulmonary dysplasia, and length of stay. However, infants exposed to maternal substance use had lower rates of respiratory distress syndrome (RDS). (Table)
Conclusion(s): Preliminary data showed that preterm infants’ less than 30 weeks’ gestation born to substance-using mothers were more likely exposed to maternal pre-eclampsia and maternal mood disorder diagnoses, needed advanced resuscitation in the delivery room including intubation, but less rates of RDS. Data collection is ongoing to verify these results. More research is needed to guide appropriate care for preterm infants exposed to drugs prenatally.