Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 1: Lung US - BPD
291 - Prediction of Adverse Outcome at One Hour of Age in Preterm Infants Less Than 30 weeks Gestational Age
Publication Number: 291.344

Michael Price, MD (he/him/his)
Fellow
University of Texas Southwestern Medical School
The University of Texas Southwestern Medical Center
Dallas, Texas, United States
Presenting Author(s)
Background: Despite advances in care, Bronchopulmonary Dysplasia (BPD) causes significant morbidity and mortality. Early identification of infants destined for adverse outcome would allow timely intervention in the most vulnerable infants. Current predictors are validated at day three of life, and none utilize blood gas results.
Objective:
We hypothesized that an early elevated ratio of respiratory severity score (RSS) to PCO2 would be associated with adverse outcome in infants less than 30 weeks gestational age (GA).
Design/Methods: We conducted a single-center retrospective review (2018-2020) of 265 infants born < 30 weeks GA that were on any respiratory support at birth. Exclusion criteria included congenital anomalies, death by 24h of life, and those on comfort care. The study group was randomly split into training (67%) and validation cohorts (33%). In addition to demographics, data on PCO2, respiratory support, mean airway pressure (MAP), and fraction of inspired oxygen (FiO2) at 1h (first blood gas by 1h of life) and 24h and day of life 3, 5, and 7 were recorded. The primary outcome was death or moderate to severe BPD at 36 weeks postmenstrual age (PMA). RSS was calculated as FiO2 x MAP. The primary dependent variable was the ratio of the RSS to PCO2. Log transformation of continuous variables was used to normalize data. Chi-square or the Fisher Exact Test was used for categorical variables and t-Test for continuous variables. Univariate and multivariate logistic analyses were performed, correcting for the effects of GA. Area Under the Curve-Receiver Operator Curve (AUC-ROC) was used to test the predictive model.
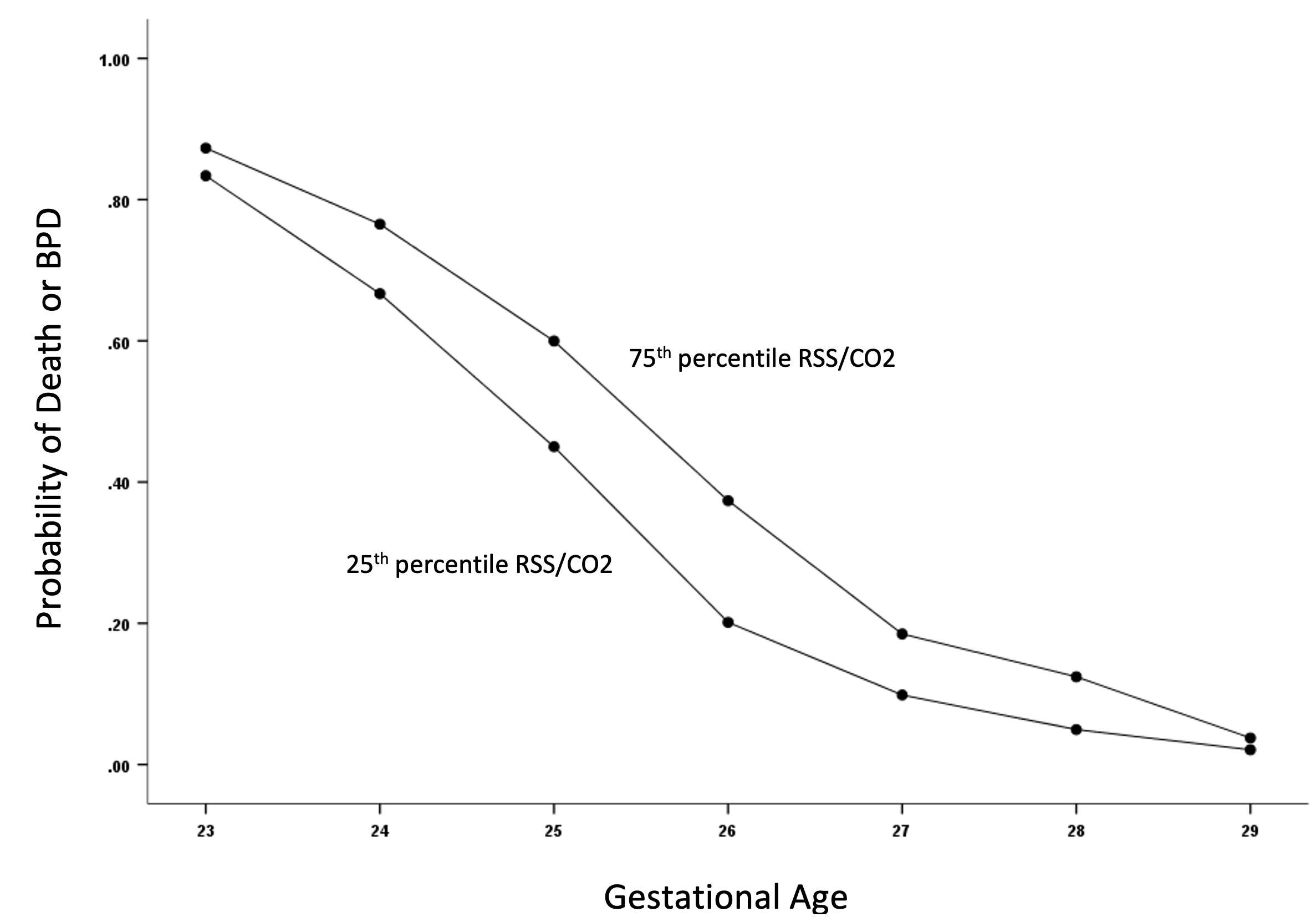
Results: Using univariate analysis at 1 and 24h in the validation cohort, Log10RSS/PCO2 was higher in infants with adverse outcome (P< 0.01). As expected, the ratio was negatively correlated to GA. Multivariate analysis controlling for GA showed an odds ratio (OR) of 6.33 (95% CI 2.11, 18.92, P < 0.01) at 1h hours and 4.21 (1.07, 16.70, p = 0.04) at 24h of life. ROC curves for RSS/PCO2 showed an AUC of 0.865 at 1h and 0.806 at 24h. Analysis of the validation cohort confirmed the association of RSS/PCO2 to adverse outcome at both 1h and 24h. A predictive model for the probability of adverse outcome using 25th and 75th percentile RSS/PCO2 at 1h was developed at each gestational age.
Conclusion(s):
In infants < 30 weeks GA on respiratory support, RSS/PCO2 at 1h of life is associated with death or moderate-severe BPD at 36 weeks PMA. These results will help identify patients at highest risk of developing adverse outcome and could be used as an inclusion criterion for clinical trials.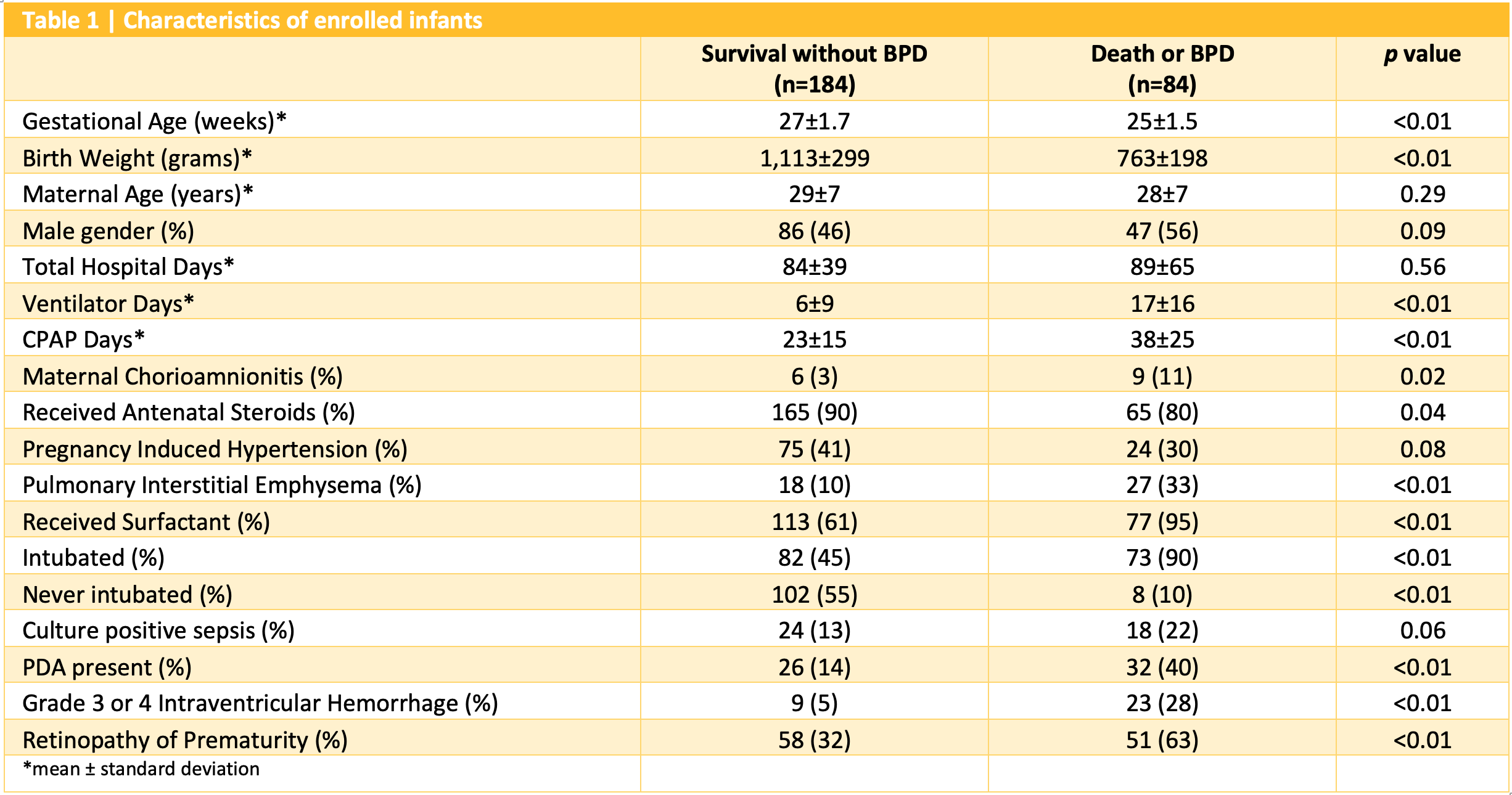
.png)
