Neonatal Quality Improvement
Neonatal Quality Improvement 3
731 - Improving Communication in Neonatal Emergencies by Establishing a Neonatal Resuscitation Team (NRT) in a Community Hospital setting
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 731
Publication Number: 731.342
Publication Number: 731.342
Johanna M. Calo, Weill Cornell Medicine, West New York, NJ, United States; Priyanka Tiwari, Weill Cornell Medicine, New Hyde Park, NY, United States; Aimee Parow, Weill Cornell Medicine, New York, NY, United States; Barbara Alba, NewYork-Presbyterian Komansky Children’s Hospital, New York, NY, United States; Cynthia Isedeh, Weill Cornell Medicine, New York, NY, United States; Carolyn Ochoa, Weill Cornell Medicine, Jersey City, NJ, United States; Bridget O'Hara, Weill Cornell Medicine, Hoboken, NJ, United States; Margaret V. Darko, Weill Cornell Medicine, New York, NY, United States; Szilvia Nagy, NewYork Presbyterian, New York, NY, United States; Julia Cron, Weill Cornell Medicine, Guilford, CT, United States; Snezana Nena Osorio, Weill Cornell Medical College, New York, NY, United States; Lyubov Osagie, NewYork-Presbyterian Morgan Stanley Children's Hospital, Staten Island, NY, United States
- JC
Johanna M. Calo, MD (she/her/hers)
Assistant Professor of Pediatrics
Weill Cornell Medicine
West New York, New Jersey, United States
Presenting Author(s)
Background: According to the NRP, most newborns make the transition to extrauterine life without intervention. However, 2% of term newborns require intubation and 1-3 babies per 1,000 births will need extensive resuscitation, including CPR. Because the need for assistance cannot always be predicted, obstetric and neonatal teams need to have effective communication to provide these lifesaving interventions quickly and efficiently.
Objective: To increase the number of appropriate emergency alerts and notifications to the Neonatal Resuscitation Team (NRT) at a community hospital affiliated with a tertiary medical center, to >50% and increase the percentage of NRT attendance at high-risk deliveries to >75% by July 2023.
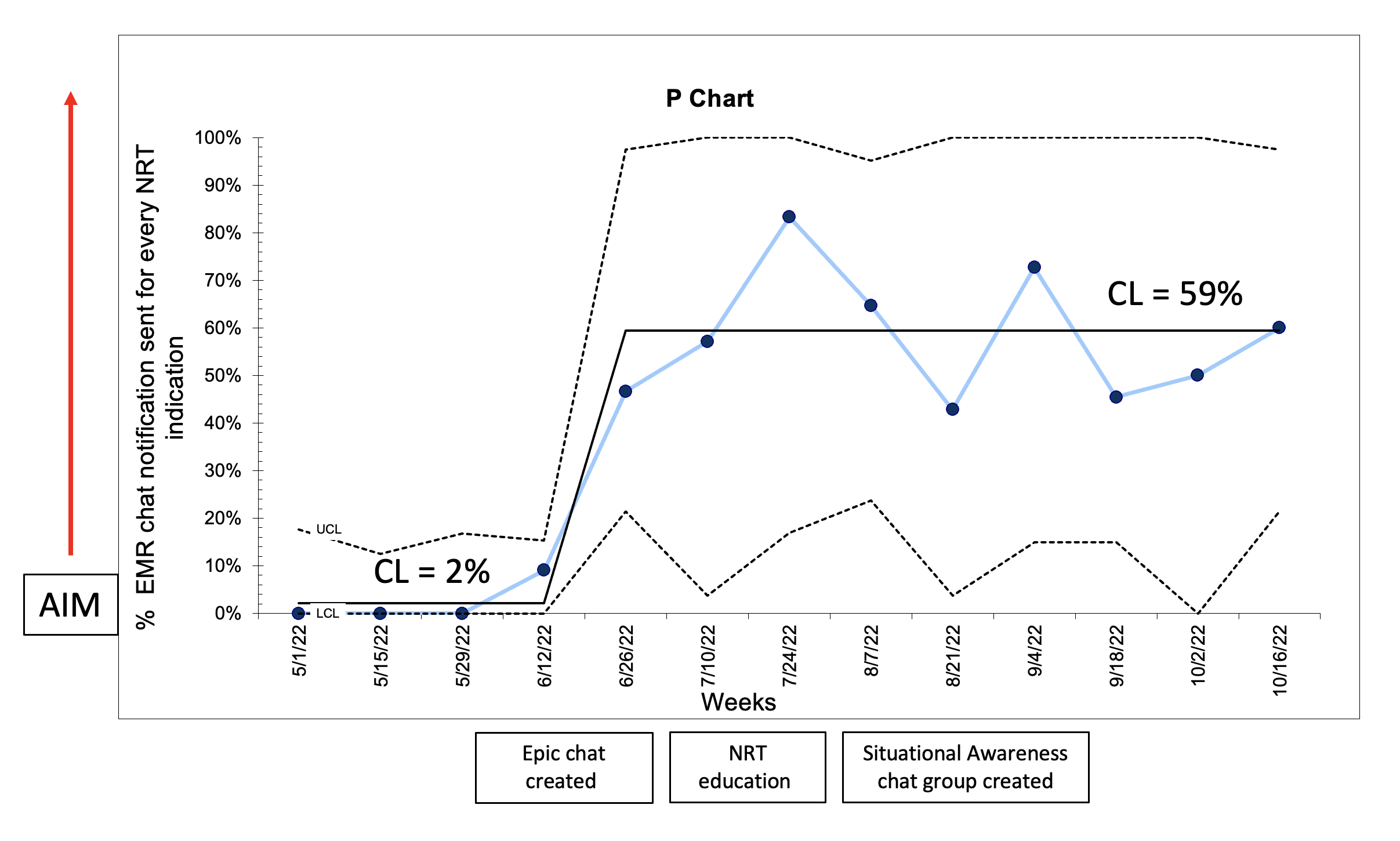
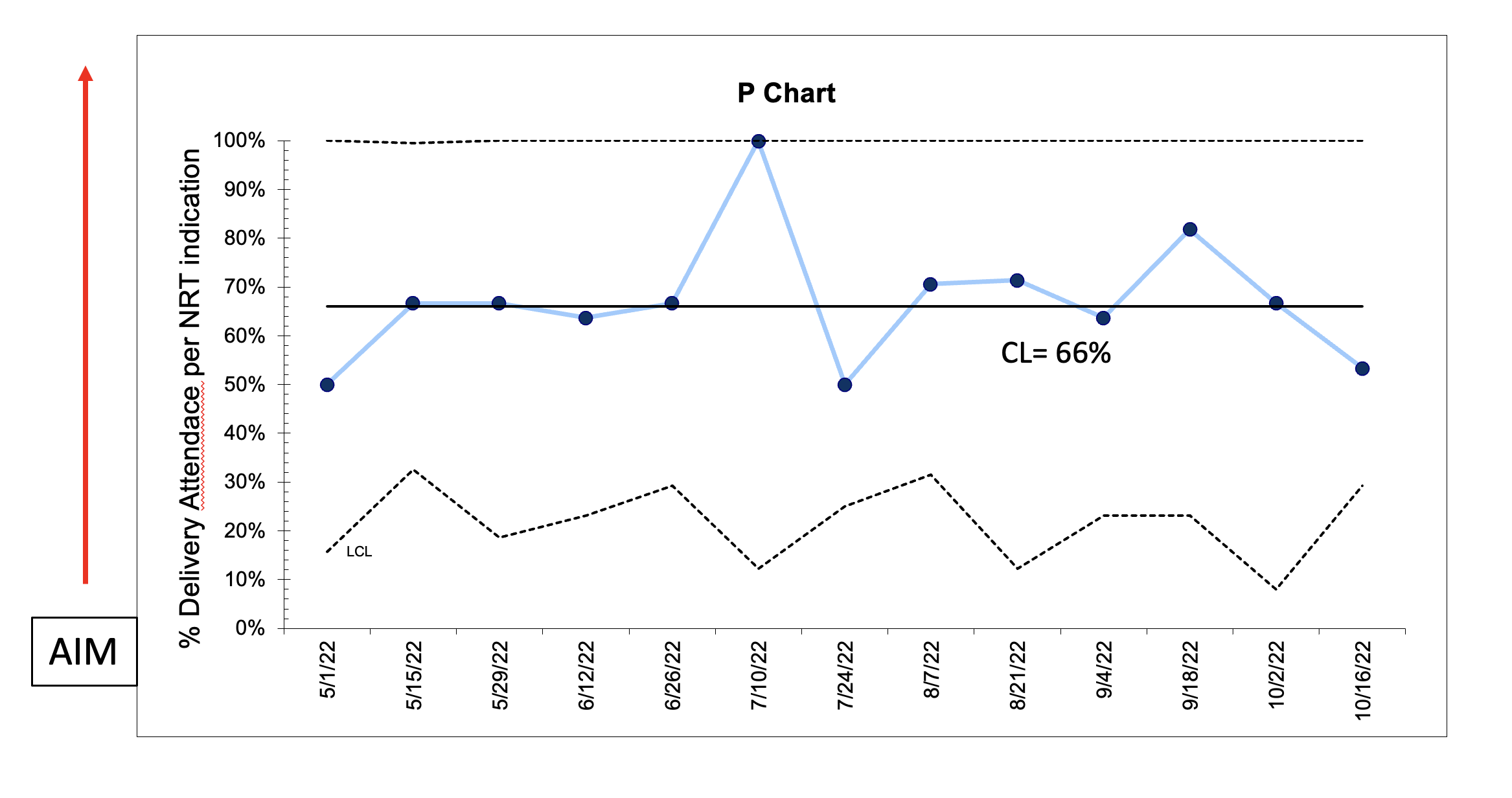
Design/Methods: This ongoing QI study utilized the Model for Improvement with a series of sequential interventions. A clinical process map was created to include indications for delivery room (DR) attendance (Fig 1). Baseline data were collected from May 1 to June 18, 2022. The following family of measures were used: number of deliveries with NRT indications for delivery room attendance (process), number of electronic medical record (EMR) chat notifications generated (outcome) and number of deliveries with NRT attendance (outcome). Our balance measure was adverse events in the NICU while the NRT team is in the DR. Statistical process control charts (P-charts) were used to display and analyze data. API rules were applied to detect special cause variation and run chart rules were applied to detect signal of change.
Results: A total of 941 maternal charts were reviewed for any indications for DR attendance by the NRT. We improved NRT notification via EMR chat from 2% to 59% (figure 2). However, the delivery room attendance remained unchanged at 66% (figure 3). There were no NICU adverse events while NRT team was in the delivery room.
Conclusion(s): The creation of a process map to alert the NRT was effective at increasing the number of appropriate emergency notifications but has not yet shown an increase in the attendance of the NRT at appropriately indicated deliveries. Next steps include activation of a NRT broadcast alert system which will allow all members of the NRT to be notified simultaneously.
.png)