Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 1: Lung US - BPD
290 - Tidal volumes of ventilated extreme premature infants in the first 4 weeks of life and development of bronchopulmonary dysplasia
Publication Number: 290.344
- MC
Milenka Cuevas Guaman, MD (she/her/hers)
Assistant professor
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background:
Bronchopulmonary dysplasia (BPD) is a major complication of extreme premature infants (EPI). Volume-targeted ventilation (VTV) is useful in preventing BPD, with volume-guarantee ventilation (VGV) being a preferred mode. Available data to guide the tidal volumes (TV) prescribed for EPIs after the 1st week of life is limited. However, larger TV could cause volutrauma and increase the risk of BPD.
Objective:
To determine the association between recorded TV (cc/kg) of EPIs on days of life (DOL) 7, 14, 21 and 28 and death and/or BPD at 36 weeks PMA as defined by the Vermont Oxford Network.
Design/Methods:
Single-centered, retrospective cohort review of medical records of premature infants less than 28 weeks admitted to a Level 4 NICU from January 2012 to December 2021. Data abstracted included: demographics, maternal and birth data, and ventilator data of VGV mode and respiratory severity score (RSS) at DOL 7, DOL 14, DOL 28 until death or discharge. Mixed-effects linear regression models were fit to make unadjusted comparisons of TV for patients experiencing versus not experiencing BPD and a BPD-death composite event, as well as to make these comparisons after controlling for RSS at each time point. A first-order autoregressive covariance structure was used for the mixed-effects linear regression models in order to accommodate the correlation between repeated TV measurements over time for the same patient.
Results:
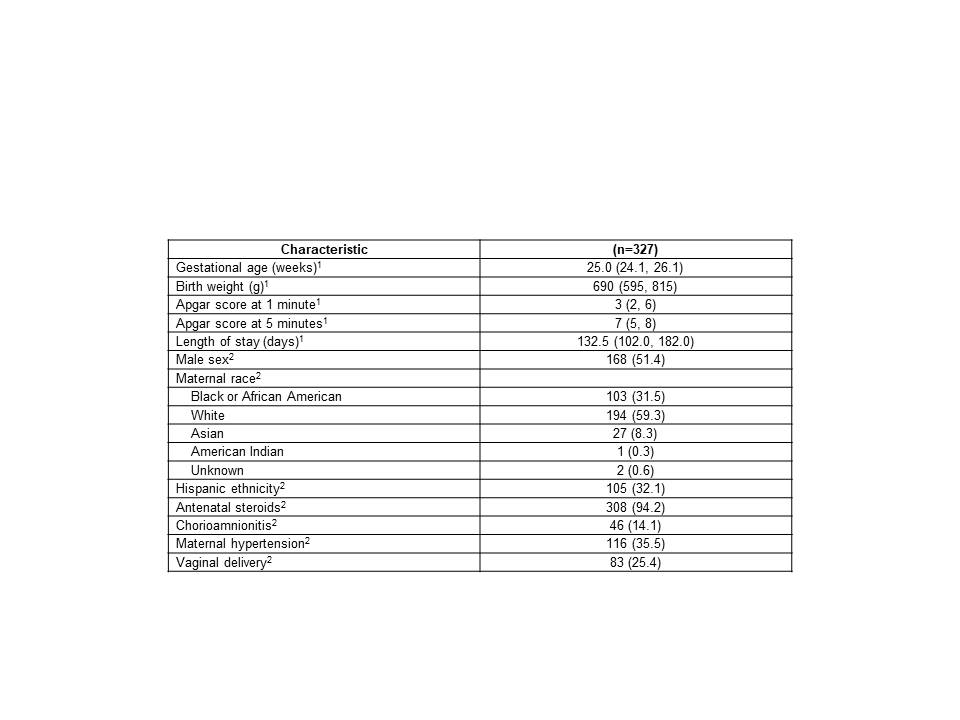
A total of 583 tidal volume measurements over the first 28 DOL from 327 patients were analyzed. 199 (34.1%) tidal volume measurements were obtained for DOL 7, 159 (27.3%) for DOL 14, 119 (20.4%) for DOL 21 and 106 (18.2%) for DOL 28. Of the 327 patients, 227 (69.4%) experienced BPD and 261 (79.8%) experienced BPD-death. Table 1 summarizes the characteristics of the 327 patients.
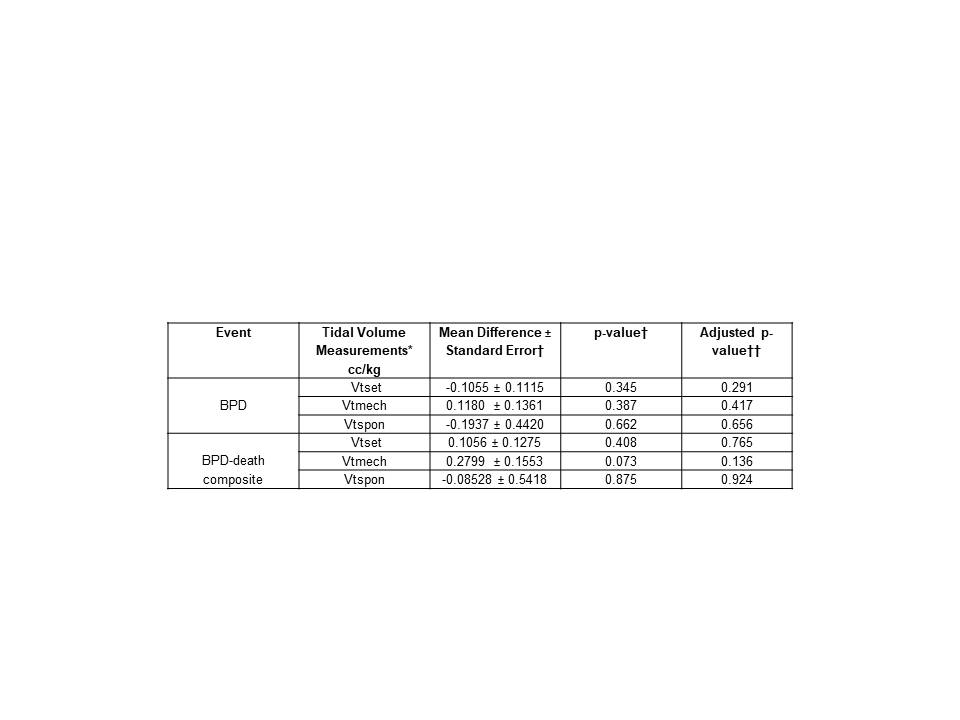
Vtmech was marginally higher (0.2799 ± 0.1553 cc/kg higher, p = 0.073) for those experiencing the BPD-death composite event after controlling for the corresponding DOL. TV measurements over the first 28 DOL for those experiencing versus not experiencing BPD or the BPD-death composite event did not differ significantly after controlling for the corresponding DOL. ± RSS (Table 2).
Conclusion(s):
In the above study, there was no association between recorded TV (cc/kg) of EPIs during the first 28 DOL and BPD or BPD-death. As ventilator-induced lung injury increases the risk of BPD/death in EPIs, further prospective studies are warrant, as well as addressing other ventilator variables.