Neonatal Quality Improvement
Neonatal Quality Improvement 4
742 - Decreasing Rates of Post-Operative Hypothermia in a Level IV NICU: A Quality Improvement Project
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 742
Publication Number: 742.343
Publication Number: 742.343
Tara Glenn, University of California, San Diego School of Medicine, San Diego, CA, United States; Branden Engorn, Rady Children's Hospital San Diego, San Diego, CA, United States; Elle Heath, Rady Children's Hospital San Diego, Virginia Beach, VA, United States; Todd Chamoy, Rady Children's Hospital San Diego, La Mesa, CA, United States; Megan L. Hedges, Rady Children's Hospital San Diego, Encinitas, CA, United States; Gloria w. Hwang, Rady Children's Hospital San Diego, san diego, CA, United States; Amanda Green, Rady Children's Hospital San Diego, Pauma Valley, CA, United States; Daniella Witt, Rady Children's Hospital San Diego, San Diego, CA, United States; Michael Van Gorder, Rady Children's Hospital San Diego, San Diego, CA, United States; Laurel Moyer, Rady Children's Hospital/University of California San Diego, San Diego, CA, United States; Peggy Grimm, Rady Children's Hospital San Diego, San Diego, CA, United States

Tara Glenn, MD (she/her/hers)
Assistant Professor
University of California, San Diego School of Medicine
San Diego, California, United States
Presenting Author(s)
Background: All infants, especially premature infants, are at risk for hypothermia during operative procedures. Hypothermia leads to metabolic and physiologic derangements and is associated with increased morbidity and mortality. Quality improvement methodology can be useful in decreasing instances of post-operative hypothermia in this vulnerable population.
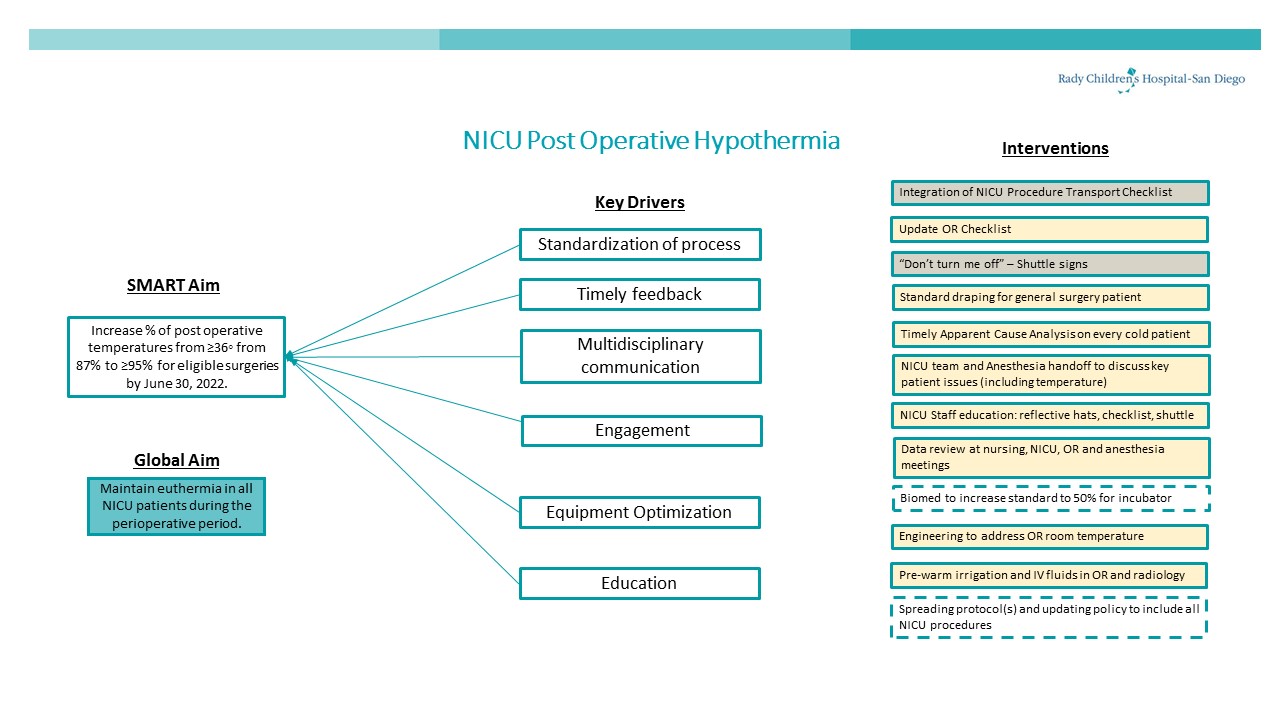
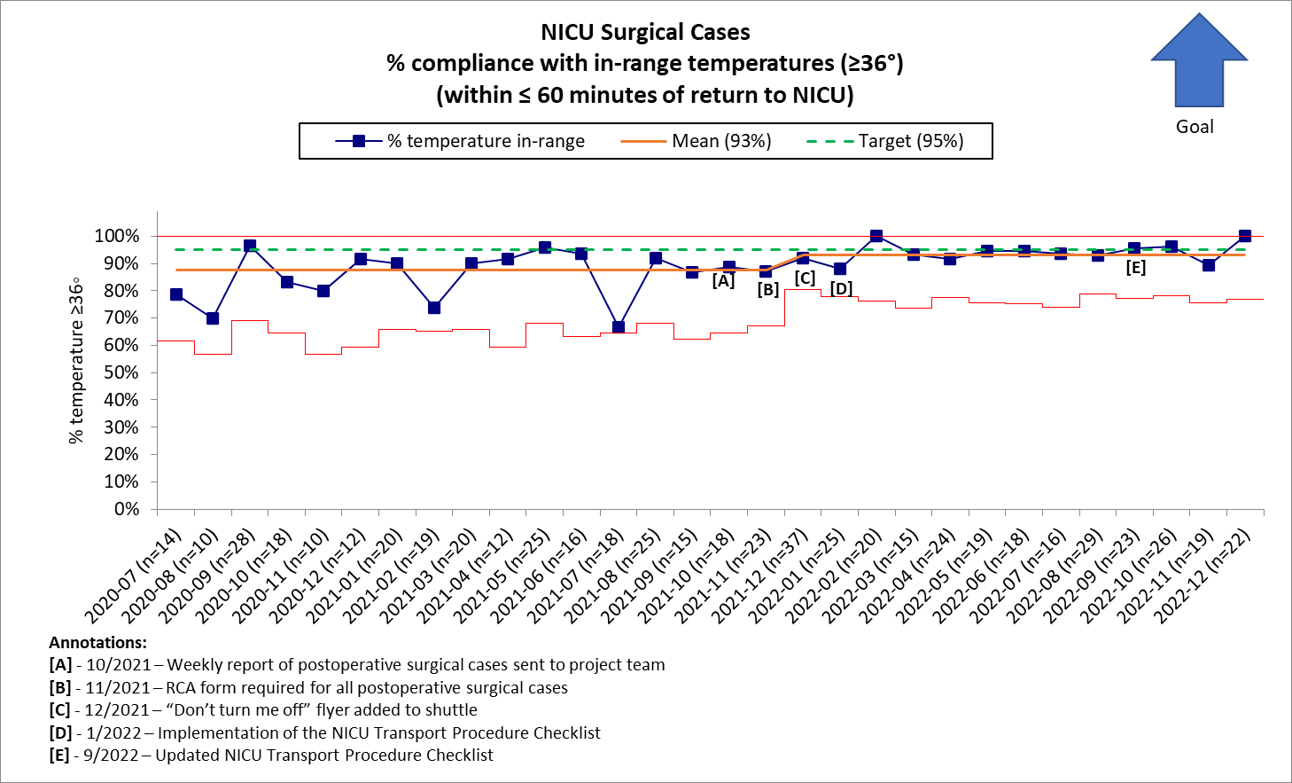
Objective: Increase the percentage of NICU patients with post-operative temperatures ≥36° from 88% to ≥95% for eligible surgeries by June 30, 2022.
Design/Methods: An interdisciplinary, team was formed with key stakeholders. We used the Model for Improvement with Plan-Do-Study-Act cycles to achieve our aim. Additional measures were collected and analyzed using pareto charts including surgical specialty. We created process maps for surgical procedures to identify areas for improvement. We then developed and modified a universal checklist to increase reliability and adherence to standards. Interventions included use of thermal hat, giraffe shuttle with radiant warmer, chemical warmer, optimizing draping and irrigation techniques, use of bair hugger, and increase in OR room temperature. To increase compliance with processes we used flyers on the shuttle and in the OR. An apparent cause analysis was undertaken on each cold infant to identify gaps in procedure and areas for improvement.
Results: Baseline data from July 2020 to June 2021 revealed a rate of 88% of post-operative temperatures ≥36° in eligible NICU surgeries. In December 2021, the data supported a special cause variation with a centerline shift to 93%. This shift indicates an increasing trend in the desired direction. Data analysis continued to show the most common surgeries associated with hypothermia were general surgery and otolaryngology, both of which make up a large portion of NICU OR cases in general. There was no increase in hyperthermia.
Conclusion(s): This QI project was the second project at this institution focused on improving rates of post-operative hypothermia. Engagement of key stakeholders coupled with integration of high reliability processes such as the checklist are essential to success of this QI work.