Neonatal Follow-up
NICU Follow Up and Neurodevelopment 5: Impact of Parents and Social Determinants of Health
158 - Social Determinants of Health and Language Outcomes in Preterm Infants with Public and Private Insurance
Publication Number: 158.363
.jpg)
Arya S. Batta, MD (she/her/hers)
Neonatal Fellow
Women & Infants Hospital of Rhode Island/ Brown University
Providence, Rhode Island, United States
Presenting Author(s)
Background: Both prematurity and public insurance (a surrogate marker for social determinants) are known to be associated with increased risk for language delay. There is a limited understanding, however, of the contribution of social determinants of health on the language outcomes of preterm infants.
Objective:
To evaluate associations of specific maternal social determinants of health on 18-24 month language outcomes of premature infants with public and private insurance.
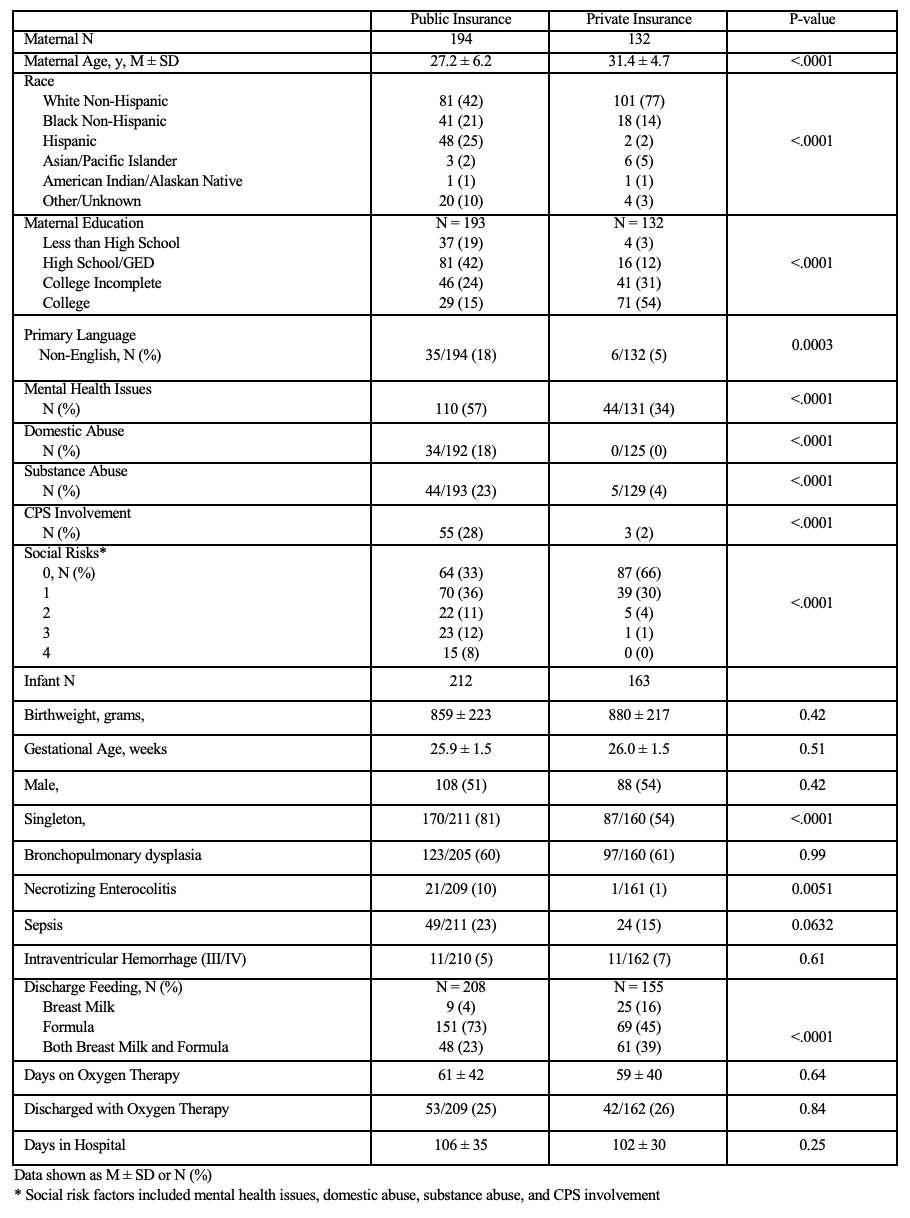
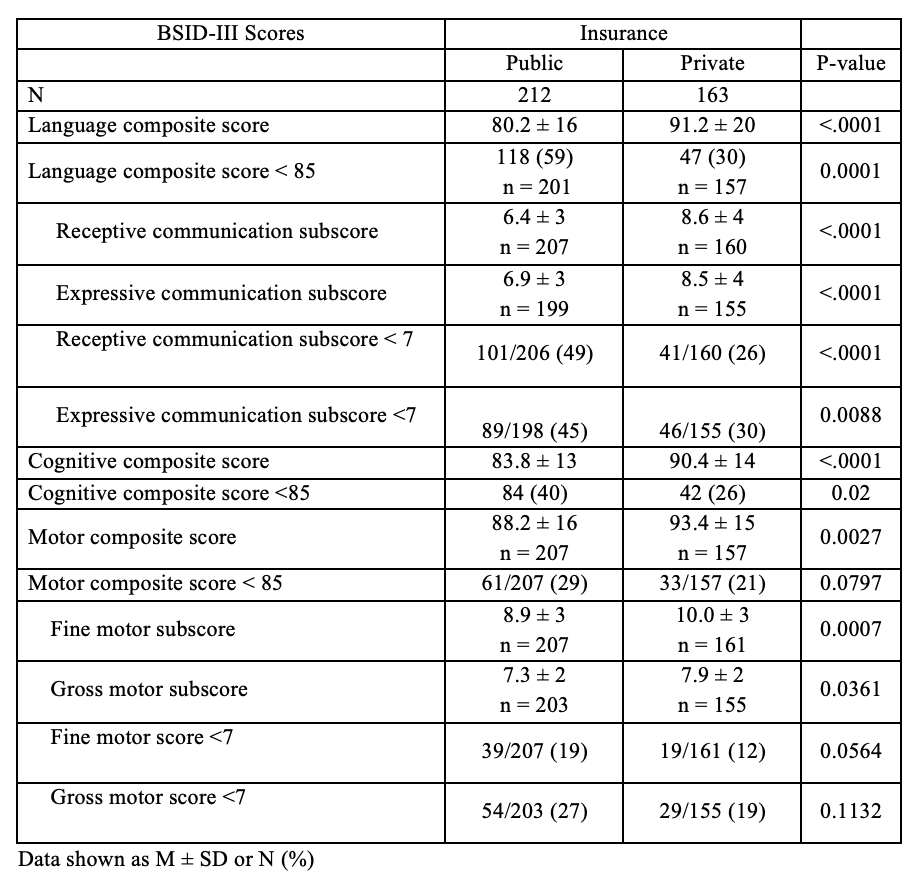
Design/Methods: This is a single center, retrospective analysis of neonates born at ≤ 28 weeks gestation. Maternal demographic data and infant characteristics and morbidities were collected, and the Bayley Scales of Infant and Toddler Development III (BSID-III) was administered at 18-24 months corrected age. The primary outcome was BSID-III language scores of < 85. Insurance was the main effect variable, with all other variables being a control variable/covariate. Bivariate analyses and multivariate logistic regression analyses were used to compare public and private insurance study groups.
Results:
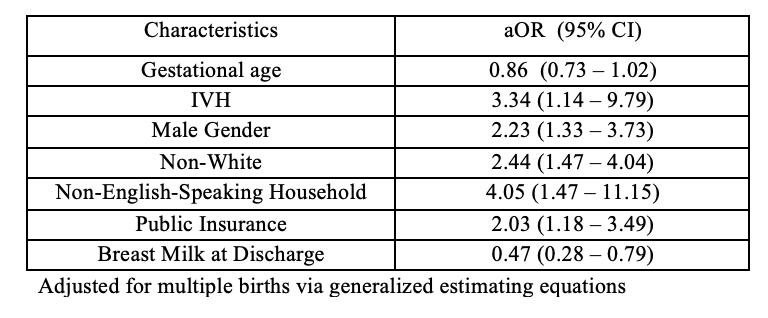
Social determinants of health were highly associated with public insurance. Mothers with public insurance were noted to have significantly younger maternal age, higher rates of non-White race, lower level of education, higher rates of non-English as primary language, and higher rates of psycho-social risk factors. In regression analysis, non-White race (aOR 2.4, 1.47-4.04), non-English speaking household (aOR 4.05,1.47-11.15) and public insurance (aOR 2.03,1.18-3.48) significantly increased the odds of having a language composite score of < 85 (aOR 2.03,1.18-3.48) whereas higher gestational age (aOR 0.86, 0.73-1.02) and breast milk (aOR 0.47, 0.28-0.79) were protective.
Conclusion(s): Social determinants of health were prevalent in our NICU population indicating a need to be identified and addressed early in order to optimize language outcomes of preterm infants. Preterm infants with public insurance combined with specific social determinants of health represent an especially vulnerable population. Providers have an opportunity to reshape health-care protocols and policies to address not only medical, but also the social-environmental risk factors impacting on developmental outcomes.