Neonatal Pulmonology
Neonatal Pulmonology 3: BPD Clinical and Translational
276 - Using noninvasively collected oral secretions to monitor respiratory health and predict BPD risk in premature neonates
Publication Number: 276.341
.jpg)
Saima Ahmed
PhD Student
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Despite decreasing rates of invasive ventilation, infants with a gestational age of < 32 weeks remain at high risk for bronchopulmonary dysplasia (BPD), and with the transition to non-invasive ventilation, easily accessible body fluids as sources of biological information are urgently needed to track lung development and better understand or predict disease risk.
Objective: We hypothesize that oral secretions (OS) can be used in lieu of tracheal aspirates (TA) as a reliable, non-invasively collected body fluid for longitudinal health monitoring in preterm infants and prediction of BPD risk.
Design/Methods:
Using an established data and sample biorepository, we applied our sample-sparing, high throughput liquid chromatography/mass spectrometry proteomics technology to compare the OS and TA proteomes of preterm newborns < 32 weeks gestational age (GA) (mean GA = 27.8 weeks) admitted to the Neonatal Intensive Care Unit (NICU), some of whom developed BPD.
Results:
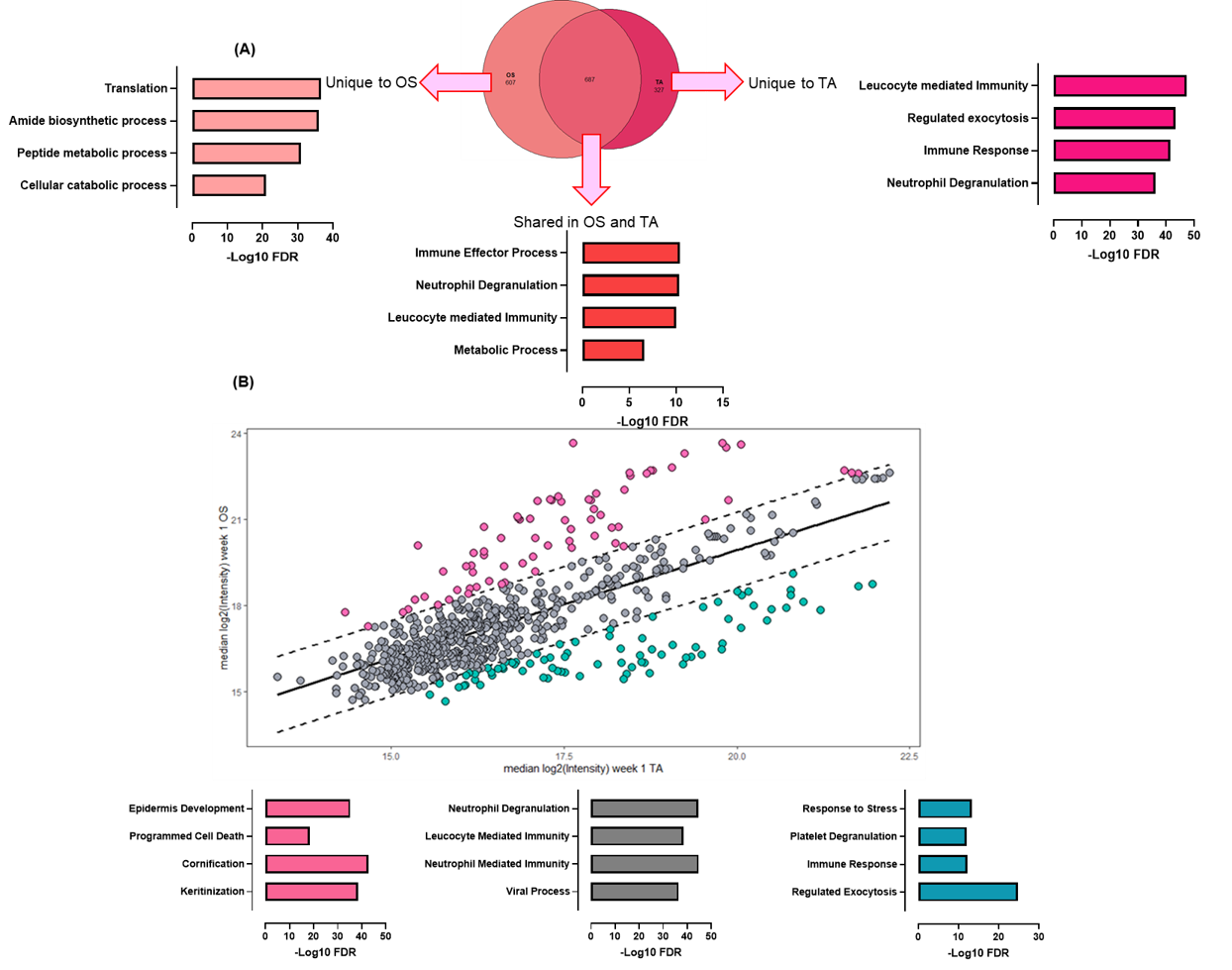
We found 687 overlapping proteomic signatures between OS and TA collected in the first week of life (WOL) belonging to pathways involved in immune effector processes (False Discovery Rate, FDR 4.15e-11), neutrophil degranulation (FDR 4.47e-11), leukocyte mediated immunity (FDR 1.02 e-10), and metabolic processes (FDR 2.5 e-07) (Figure, A). A correlation analysis of the OS and TA proteomes showed several proteins highly correlated belonging to biological pathways related to immunity and viral processes (Figure, B). To determine associations between the OS proteome and eventual development of BPD, we compared early life (WOL 3) OS proteomes from 17 infants, 8 of whom developed BPD. We identified 37 significant proteins differentiating infants who developed BPD vs not, including 6 metabolic and 7 immune proteins. Ten of the 37 proteins (SERPINC1, CSTA, BPI, S100A11, ANXA1, ANXA8L1, ANXA8, TKT, TPP2, PDCD6) had previously been linked to BPD or other prematurity-related lung disease pathophysiology from blood sample or TA investigations, but not OS.
Conclusion(s):
OS are a readily accessible and convenient body fluid in frail newborns and their proteome reflects that of TA suggesting that OS can be used as a noninvasive alternative for respiratory health monitoring of high-risk preterm infants. Small OS samples are amenable to high throughput omics and can be used to identify biologically plausible OS proteomic markers predictive of future BPD risk.