Emergency Medicine: All Areas
Emergency Medicine 11
479 - Factors Associated with Caregiver Refusals for Children Left at Scene by Emergency Medical Services (EMS)
Publication Number: 479.31

Kristen E. Johnson, MD (she/her/hers)
Clinical Associate
Childrens National Medical Center
Fairfax, Virginia, United States
Presenting Author(s)
Background:
Almost one third of pediatric 911 calls result in non-transport by Emergency Medical Services (EMS). In some cases a caregiver refuses transport, while in other cases EMS providers advise that transport is not necessary. There is limited information regarding the proportion of pediatric non-transport due to caregiver refusals. It is unknown whether demographic, encounter, or agency factors are associated with caregiver refusals.
Objective:
Our primary objective was to determine the prevalence of, and factors associated with, caregiver refusal of pediatric EMS transport. Our secondary objective was to determine how pediatric non-transport and caregiver refusals vary across EMS agencies.
Design/Methods:
We conducted a retrospective cross-sectional study with data from the national 2019 ESO Data Collaborative (a convenience sample with data from > 2,000 EMS agencies). We included 911 responses for children < 18 years. The primary outcome was caregiver refusal per EMS documentation. Descriptive data for patient dispositions were generated. Bivariable and multivariable logistic regression tested factors for association with caregiver refusal.
Results:
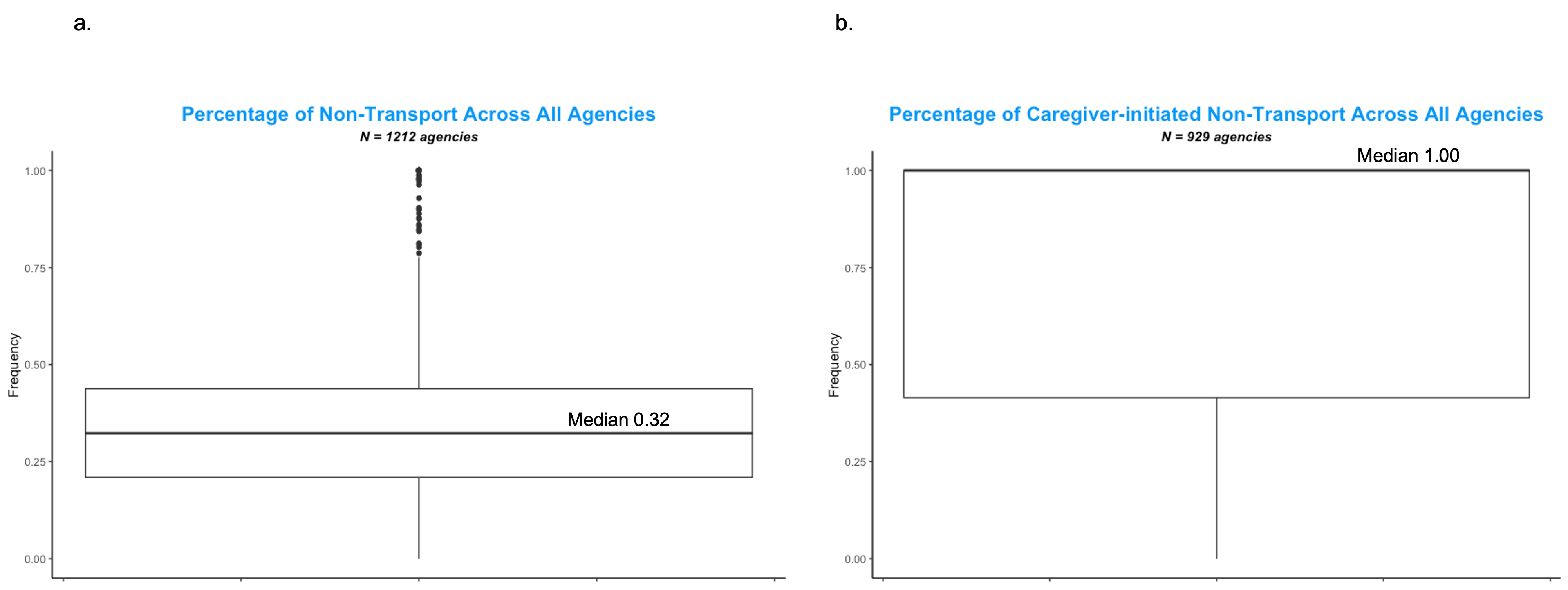
Of 333,351 eligible records, 30.8% resulted in non-transport. 70.3% of non-transport was due to caregiver refusals, with the remainder initiated by EMS (Table 1). Amongst all non-transports, caregiver refusals were most strongly associated with calls attended by a BLS clinician (aOR 1.69 [95% CI 1.49, 1.93]), originating in super-rural area (aOR 3.77 [2.97, 4.84]), and initiated by a patient/bystander (vs. healthcare provider) (aOR 1.62 [1.45, 1.80] (Table 2). Weaker positive associations with caregiver refusal were found for female gender, Black and Hispanic race/ethnicity, calls for trauma, and encounters where no injuries were identified. Encounters with complete vital signs were more likely to result in refusal 1.81 [1.69, 1.94]. When analyzed by EMS agency, there was significant variability in non-transport rates (median 32.3% [IQR 21.0–43.8%]) and, among non-transport cases, rates of caregiver refusal (median 100% [IQR 41.5–100%]).
Conclusion(s):
In this national dataset, almost a third of all children were not transported by EMS, with most non-transport due to caregiver refusal. Patient demographics, nature of the medical complaint, composition of the EMS team, and urbanicity were associated with caregiver refusals. Both rates of non-transport and caregiver refusal varied significantly among EMS agencies. Further research is needed to describe patient outcomes after non-transport and to explore reasons for EMS agency practice variability.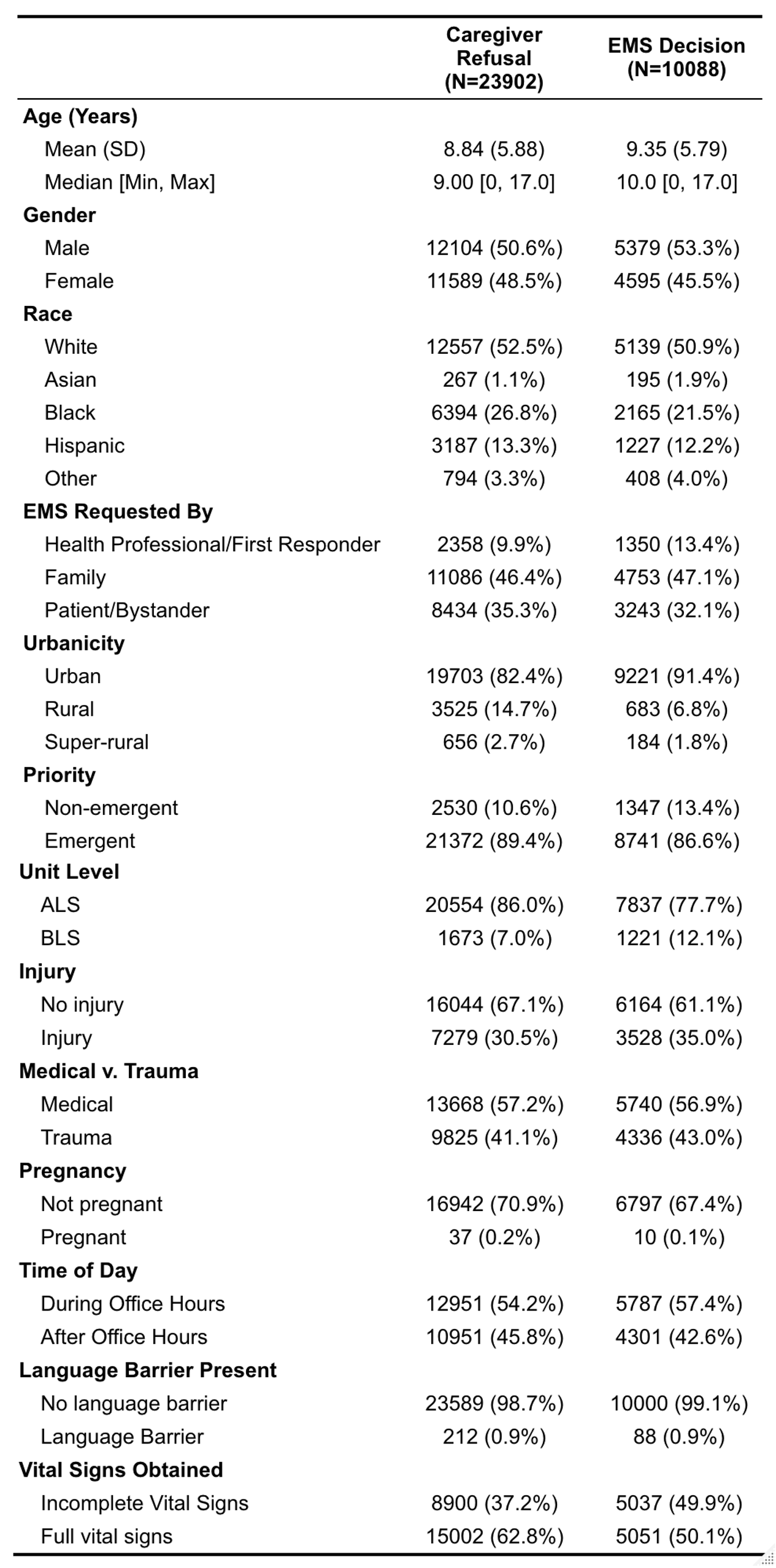
.png)