Neonatal Pulmonology
Neonatal Pulmonology 2: BPD Clinical
259 - Comparing the ability of new definitions of severe bronchopulmonary dysplasia to better predict outcomes
Publication Number: 259.34

Gangaram Akangire, MD, MS (he/him/his)
Neonatologist
Children's Mercy Hospitals and Clinics
Children's Mercy Hospital
Kansas City, Missouri, United States
Susan McAnany, MD (she/her/hers)
Neonatology Fellow
Children's Mercy Hospitals and Clinics
Overland Park, Kansas, United States
Presenting Author(s)
Co-Author(s)
Background:
BPD is the most common complication of prematurity and its incidence is increasing. The 2000 NIH Consensus definition helped to delineate severity associated with the now common classification for BPD. Later classifications for severe BPD that encompass more granular data have been proposed, but it is unknown whether one predicts mortality and long-term respiratory and growth outcomes better compared to the others.
Objective:
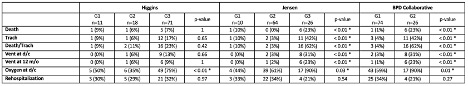
We compared three newly proposed definitions of severe BPD (Higgins, Jensen, BPD Collaborative) to determine if one better predicts morbidity and mortality associated with BPD in the first year of life. Primary outcomes included either death or need for tracheostomy. Secondary outcomes included the use of ventilator support, oxygen, diuretics, pulmonary HTN medication, and NG or GT feeds, weight gain, and rates of rehospitalization.
Design/Methods:
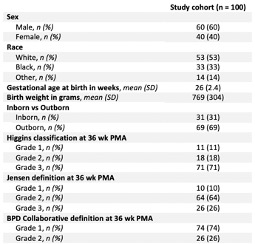
Our study population included all patients diagnosed with severe BPD from Children’s Mercy Hospital NICU that were discharged between Jan 1, 2019 and Dec 31, 2020. In-hospital and discharge outcome data were collected from EMRs after receiving IRB approval. Each patient was reclassified using the three newly proposed definitions of severe BPD (table 1) and outcomes were tested for significance using chi-square, Fisher’s exact and Wilcoxon Rank Sum tests.
Results: In our cohort of 100 infants with severe BPD, the average gestational age was 26 0/7 weeks and birthweight was 769 grams. Other demographic variables are shown in table 2. Jensen and BPD collaborative classifications for severe BPD best predicted outcomes at discharge, 6 months after discharge, and 12 months after discharge. Both groups were able to predict our primary outcomes of death (p = ≤ 0.001 for Jensen, p = 0.001 for BPD Collaborative), the need for tracheostomy (p = ≤ 0.001 for both), and death or the need for tracheostomy (p = ≤ 0.001 for both). Both also found statistical significance in use of ventilator support, use of supplemental oxygen, and use of NG or GT feeds. No classification was able to predict rehospitalization.
Conclusion(s):
Jensen and BPD collaborative definitions best predict death and respiratory outcomes up to 1 year after discharge. Our data suggest that Jensen and BPD collaborative definitions should be adopted as they better predict outcomes enabling providers to better guide families on decision-making. Replication of our single-center study in other centers is warranted before adopting more precise definitions of BPD..png)