Neonatal Neurology: Clinical Research
Neonatal Neurology 5: Clinical
111 - Clinical Use of MRI Scores of Term-Equivalent Age Brain MRI of Very Preterm Infants in the NICU
Publication Number: 111.337

Aisling A. Garvey, MB BCh BAO PhD (she/her/hers)
Neonatal Trainee
INFANT Centre, Ireland/Brigham and Womens Hospital, USA
INFANT Centre
Cork, Cork, Ireland
Presenting Author(s)
Background:
Despite advances in maternal and neonatal care, preterm infants remain at risk for adverse long-term neurodevelopmental outcomes. MRI is more sensitive than cranial ultrasound at detecting white matter injury and is increasingly being used to define preterm brain injury. Translating MRI findings into prognostic outcome, however, remains challenging.
Objective: This study aimed to improve the interpretation and clinical utility of term-equivalent age (TEA) MRIs of very preterm infants by providing the clinical team with individualized MRI reports based on a previously published scoring system.
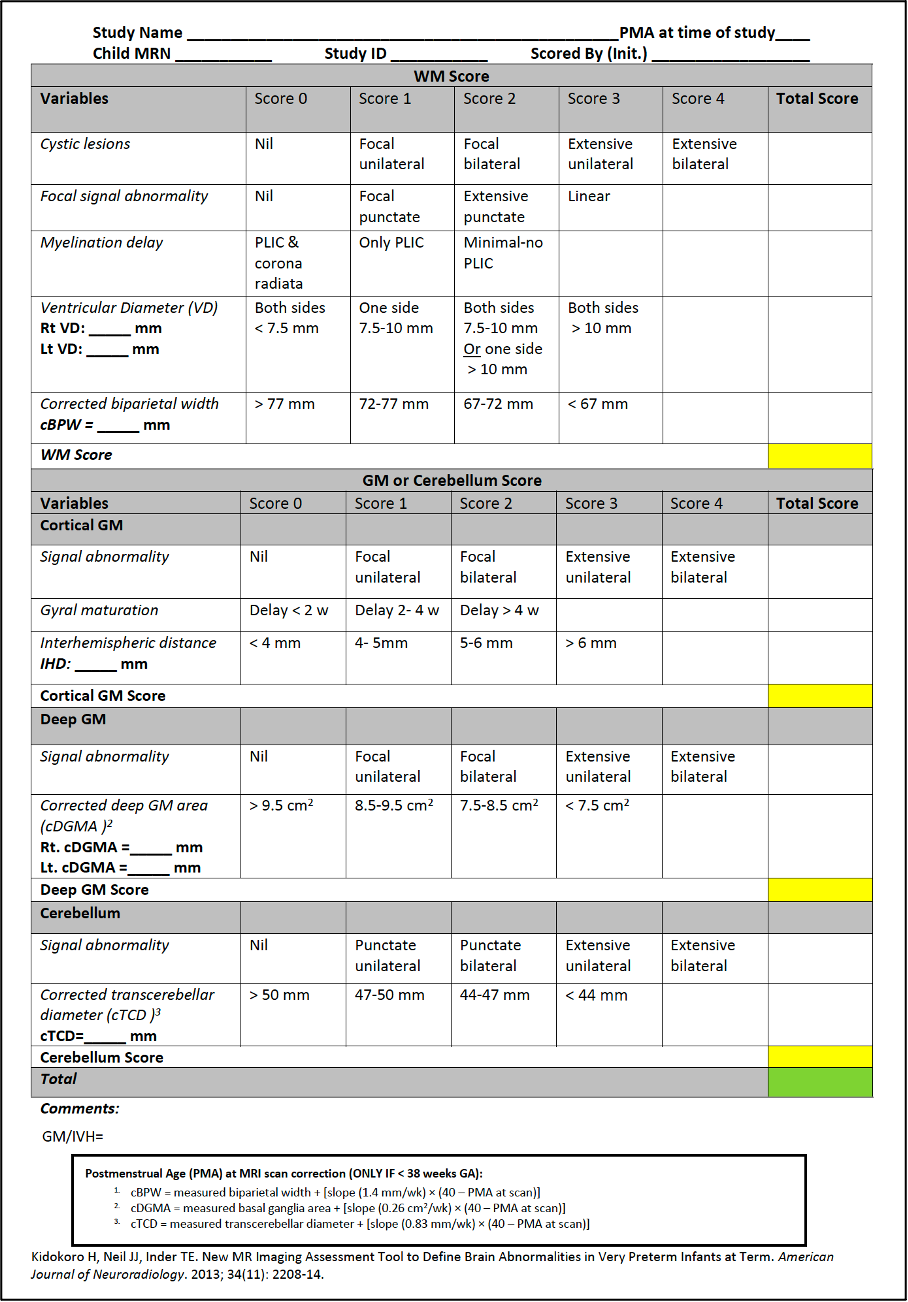
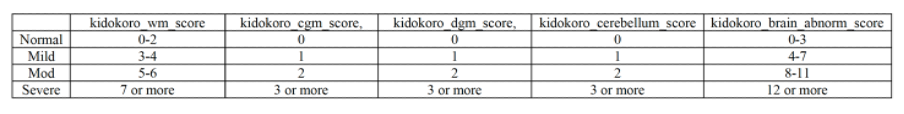
Design/Methods: This study was conducted at the Brigham and Women’s Hospital, Boston, a 66-bed tertiary neonatal intensive care unit (NICU). In our center, all infants born < 28 weeks or < 32 weeks with additional risk factors undergo an MRI at TEA. While results are reported by specialized neuroradiologists, the medical providers are the ones responsible for the interpretation of these scans and subsequent communication with parents. We anonymously surveyed medical providers. Survey included questions about the knowledge and confidence in interpreting TEA MRIs, prediction of outcome and conveying results to parents. Over a period of 4 months, all TEA MRIs were scored using a previously published scoring system and individualized reports using evidence-based outcomes were sent to providers within 24-48 hours of the MRI. Following the intervention, providers were surveyed again to determine whether they found the reports helpful.
Results:
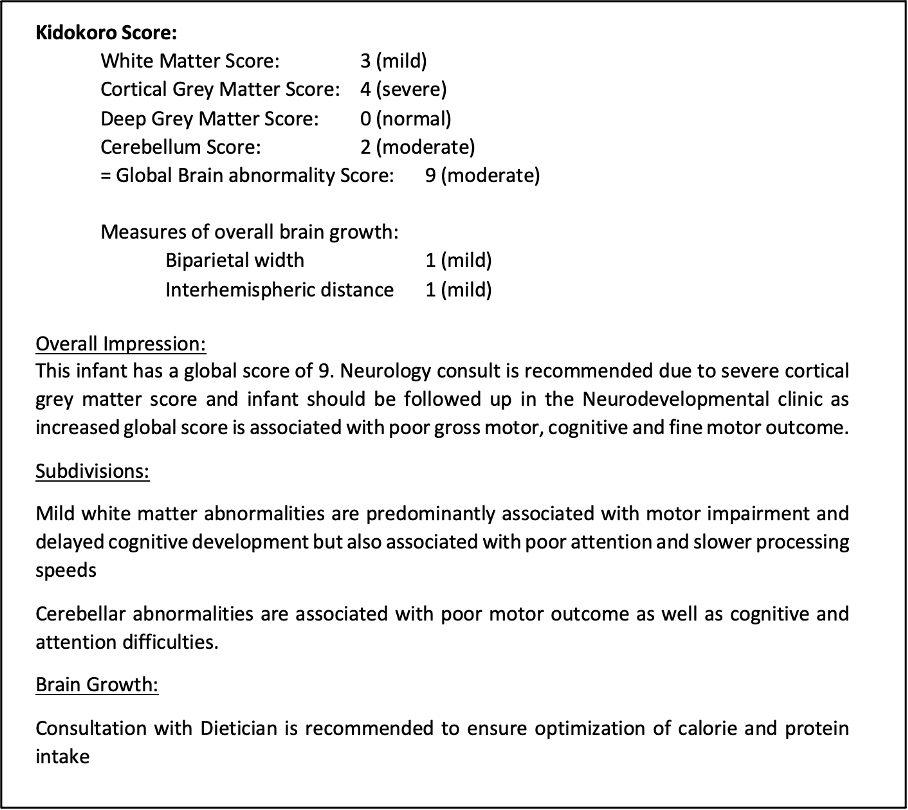
Nine medical providers were included in the initial survey, two-thirds of whom were only slightly or not confident in interpreting the MRI clinical report, how injury related to outcome and in conveying the results of the MRI to parents. During the 4-month period, 14 reports were formulated and sent to caregivers. An example of one of these reports is demonstrated in Figure 1. Following the intervention, all providers reported that the intervention was helpful and allowed for “better, more cohesive plans with families” and improved ability to interpret findings of brain growth more quantitatively and integrate this information in clinical care.
Conclusion(s):
To date, MRI scoring systems have predominantly been used in research settings. Its use in this clinical setting was feasible and provided an objective, quantifiable assessment of brain growth and injury in very preterm infants allowing for individualized reports and subsequently targeted interventions and follow-up.