Nephrology: CKD
Nephrology 6: Glomerular/Clinical and Basic Science
65 - Social Determinants of Health in Utilization of Home Urine Dipsticks in Nephrotic Syndrome
Publication Number: 65.351
Timothy Lequang, MS
Medical Student
Pennsylvania State University College of Medicine
Hummelstown, Pennsylvania, United States
Presenting Author(s)
Background:
Nephrotic syndrome (NS) relapses can be identified prior to development of clinical symptoms using home urine dipsticks (DS) for protein. In those with steroid-responsive disease, early detection and treatment of a relapse can prevent hospitalizations for symptomatic edema, acute kidney injury, infections, and other complications of active NS.
Objective:
We aimed to compare the accuracy and precision of various commercially available urine DS for protein brands to the brand used in our clinic (Siemens) and describe the characteristics of our NS population who have and do not have home urine DS.
Design/Methods:
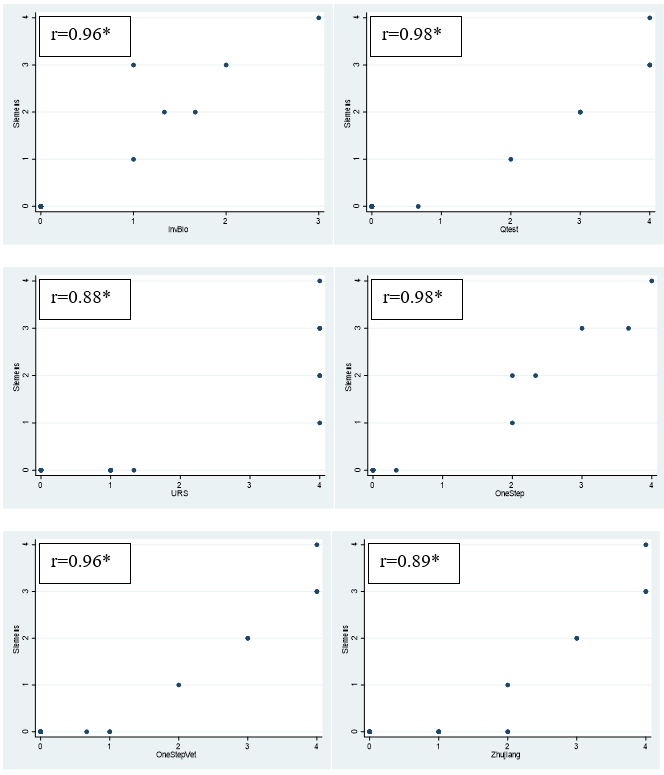
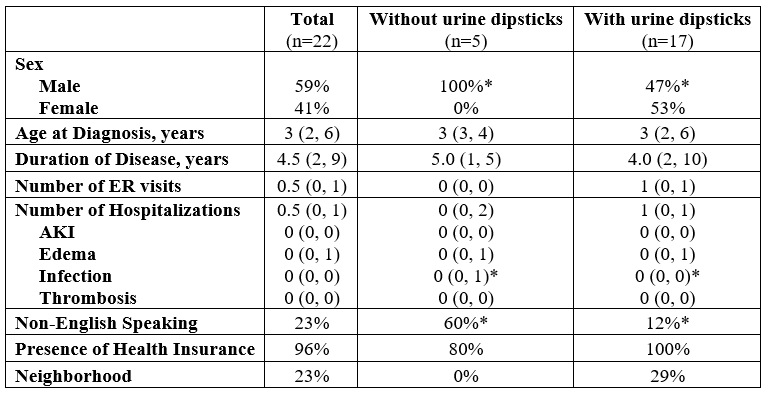
Urine samples from 23 patients seen at Penn State’s Pediatric Nephrology clinic were tested for urine protein level with 6 commercially available urine DS for protein brands with comparison to Siemens for accuracy using a pairwise correlation coefficient on the average urine protein value measured in + units on 3 repeated measures. Precision was assessed using standard deviation (STD). An electronic medical record review of patients seen within the past 6 months with a diagnosis of presumed minimal change disease (MCD) or MCD on biopsy identified 34 patients. Chi-squared and Mann-Whitney rank sum tests were used to assess factors associated with home urine DS use.
Results:
The correlation coefficient between Siemens urine DS and each of the commercially available urine DS brands ranged from 0.89 to 0.98 (p< 0.05). The average STD in urine protein level ranged from 0 to 0.3 + units with a median of 0 (interquartile range 0 to 0) + units. In those with frequently relapsing disease, a statistically significant difference in sex, hospitalizations for infection, and need for language interpretation services was noted between those who used urine DS to manage their disease versus those who did not (p< 0.05). Specifically, males were more likely to not have urine DS at home. Patients without urine DS were noted to have greater number of hospitalizations for infections, and those without urine DS at home were more likely to be patients requiring language interpretation services (p< 0.05).
Conclusion(s):
All commercially available urine DS brands that were tested had similar accuracy and precision. Pediatric nephrologists should feel comfortable recommending most brands for home monitoring of urine protein level. Non-English-speaking patients were less likely to have urine DS at home. This is a barrier that needs to be addressed as use of urine DS in those with frequently relapsing disease was associated with decreased incidence of hospital admissions for NS associated infections.