Neonatal General
Neonatal General 9: NOWS and Other Exposures
199 - Early vs late non-prescribed opioid use in pregnant individuals on medication for opioid use disorder and association with pregnancy and neonatal outcomes
Publication Number: 199.333

Laurie Delatour, MD/PhD
Resident
Boston Medical Center, Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: For individuals with opioid use disorder (OUD) in pregnancy, medication for the treatment of OUD (MOUD) is the standard of care and is associated with improved pregnancy and neonatal outcomes. The association of any continued non-prescribed opioid use on these outcomes, and the influence of early versus late non-prescribed opioid exposure, remains unexplored.
Objective:
To examine how continued non-prescribed (NP) opioid use by pregnant individuals on MOUD affects pregnancy and neonatal outcomes, and whether the effect is specific to early vs late exposure.
Design/Methods:
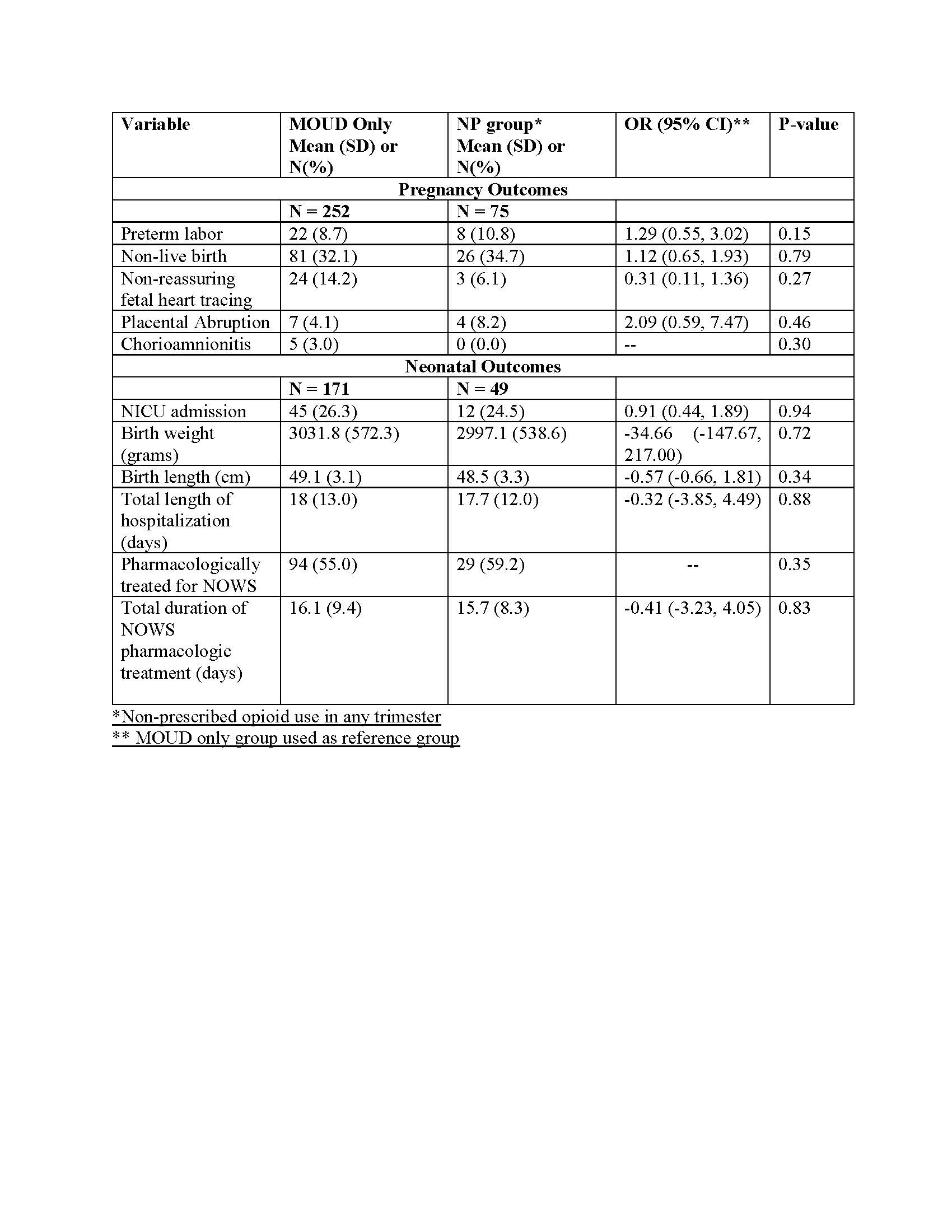
Retrospective data from mother-infant dyads born between 2014-2021 collected through the MAT-LINK project were analyzed. A subset of those with MOUD exposure only was compared with those with MOUD plus NP opioid use in any trimester, with the MOUD group as the reference. Individuals were further grouped in early (first trimester) or late (second/third) trimester cohorts to assess the effects of timing of exposure to NP opioids. The following outcomes were examined between groups: preterm labor, non-live births, non-reassuring fetal heart tracing, placental abruption, chorioamnionitis, NICU admission, birth weight, birth length, total length of hospitalization, pharmacologic treatment for NOWS, and duration of NOWS treatment.
Results:
There were 252 dyads, including 75 in NP group (47 early and 28 late trimester). There were no demographic differences between the MOUD and NP groups with the exception of more methadone treatment in the NP group (Table 1). When comparing MOUD versus the entire NP group, there were no differences in outcome measures (Table 2). When comparing the MOUD vs NP early exposure groups, there was a significant increase in the preterm labor in the NP early exposure group. When comparing the MOUD vs NP late exposure groups, there were no significant differences in outcome measures. (Table 3).
Conclusion(s): Continued non-prescribed opioid use by pregnant individuals during the first trimester is associated with an increase in preterm labor. Additional work is needed to further investigate other outcome measures potentially affected by non-prescribed opioid exposure. 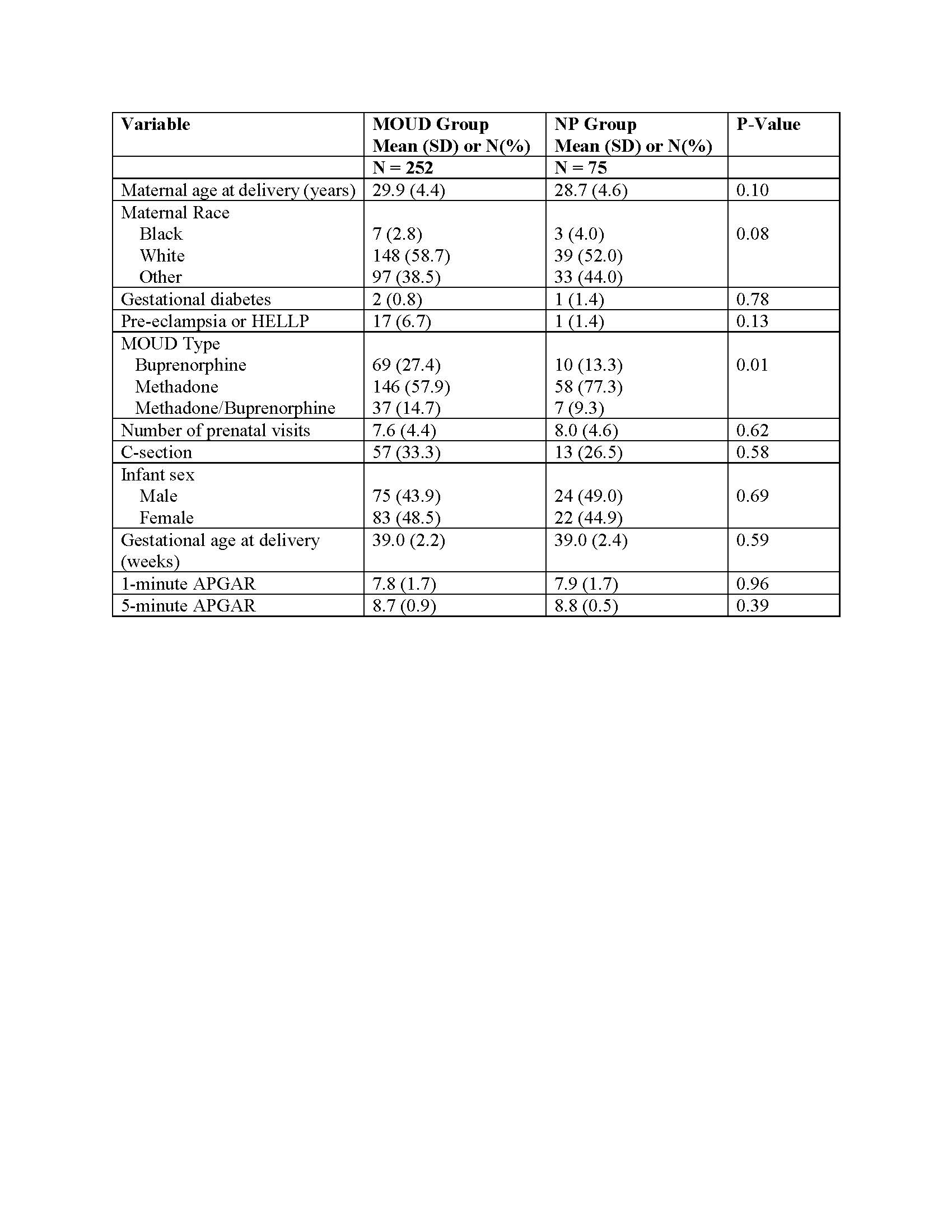
.jpg)
