Neonatal Quality Improvement
Neonatal Quality Improvement 4
739 - Behind the Screens: Using Quality Improvement to Implement Depression and Anxiety Screening in a Neonatal Intensive Care Unit
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 739
Publication Number: 739.343
Publication Number: 739.343
Sarah A. Swenson, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Delaney E. Wilton, University of Minnesota Medical School, Apple Valley, MN, United States; Maria Kroupina, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Ann Downey, Children's Hospitals and Clinics of Minnesota, Minneapolis, MN, United States; Erin Osterholm, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Kate A. Goerdt, M Health Fairview Hospital, Minneapolis, MN, United States; Megan Paulsen, University of Minnesota Medical School, Minneapolis, MN, United States

Sarah A. Swenson, MD, DPhil (she/her/hers)
Neonatal-Perinatal Medicine Fellow
University of Minnesota
Minneapolis, Minnesota, United States
Presenting Author(s)
Background: Perinatal Mood and Anxiety Disorders (PMADs) are the most common complication of childbirth and a leading cause of maternal postpartum mortality. Neonatal Intensive Care Unit (NICU) parents are not screened in primary care (PC) clinics at the American Academy of Pediatrics recommended intervals when their infants remain hospitalized, despite being at higher risk. Premature and critically ill infants exposed to parents with untreated PMADs are at higher developmental risk. Improved identification and treatment of PMADs for NICU families is essential. We aimed to implement routine PMAD screening and achieve 70% completion with referral for all parents of hospitalized NICU infants at 1, 2, 4, and 6-month intervals by January 2023. Here we present our first 5 weeks of data.
Objective: Standardize PMAD screening for NICU parents
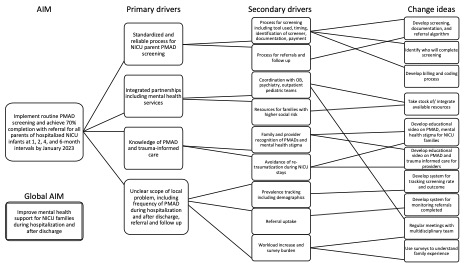
Design/Methods: Our multidisciplinary team designed a driver diagram and screening algorithm for parents with infants admitted to MHealth Fairview Masonic Children’s Hospital Level IV NICU, Minneapolis, Minnesota. Baseline data were collected from March-September 2022. We implemented screening using the Edinburgh Postpartum Depression Scale (EPDS) and anxiety subscale in October 2022. Outcome measures included rate above screening threshold and timing of mental health (MH) concern. Process measures included rate of gestational parents (GP) v. nongestational parents (NGP) screened with subgroup analysis. Balancing measures were NICU parent, social worker, and neonatologist perceptions of screening.
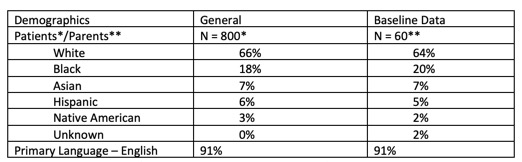
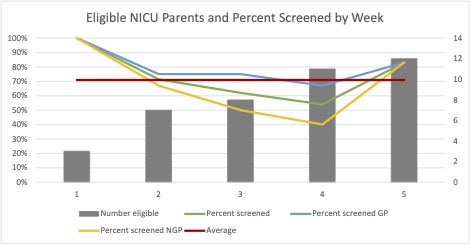
Results: We admitted approximately 800 infants with an average length of stay of 30 days during the study period. In a 6-month period prior to routine screening, 60 MH referrals were made based on clinical concerns from the NICU team (rate of 2.4 per week), occurring primarily in GP (96%) v. NGP (4%). 73% and 78% of referrals were made within 1 and 2 weeks after birth, respectively. In the first 5 weeks of screening, 71% of 41 eligible parents were screened. MH and PC referrals were made based on positive screens (rate of 2 per week). Rate of screening GP was higher than NGP (77% v. 63%). 36% of screens were positive for depression (36% GP v. 36% NGP) and 40% for anxiety (43% GP v. 36% NGP). 7% of screens identified passive suicidality with GP and NGP represented equally. Screening was viewed positively by 92% of parents and 90% of providers.
Conclusion(s): Standardized PMAD screening in NICU parents resulted in an additional 2 referrals per week, identified more NGP with MH symptoms, and was viewed positively by parents and providers.