Global Neonatal & Children's Health
Global Neonatal & Children's Health 2
639 - Prevention and Treatment of Neonatal Hypothermia through an Implementation Science Study in Jaltenango Chiapas, Mexico.
Publication Number: 639.316

Alejandro Frade Garcia, MD (he/him/his)
Fellow
Boston Children's Hospital
Miami, Florida, United States
Presenting Author(s)
Background:
Neonatal Hypothermia (NH) is a common, preventable contributing factor to neonatal morbidity and mortality, disproportionately affecting newborns in low income settings. Kangaroo Mother Care (KMC) is the preferred method to prevent NH in these settings. Yet relying on KMC as a continuous heat source is challenging. Novel infant warmers designed for low resourced settings present an important option to complement KMC. Through an implementation science study we introduced such a device into a low resource community hospital.
Objective:
We conducted a hybrid implementation science study in the community hospital of Jaltenango Chiapas, Mexico from January to November 2022. We evaluated the effectiveness of our strategy while also assessing the healthcare workers' perception of our intervention with the hypothesis that the NH rates would decrease with the intervention.
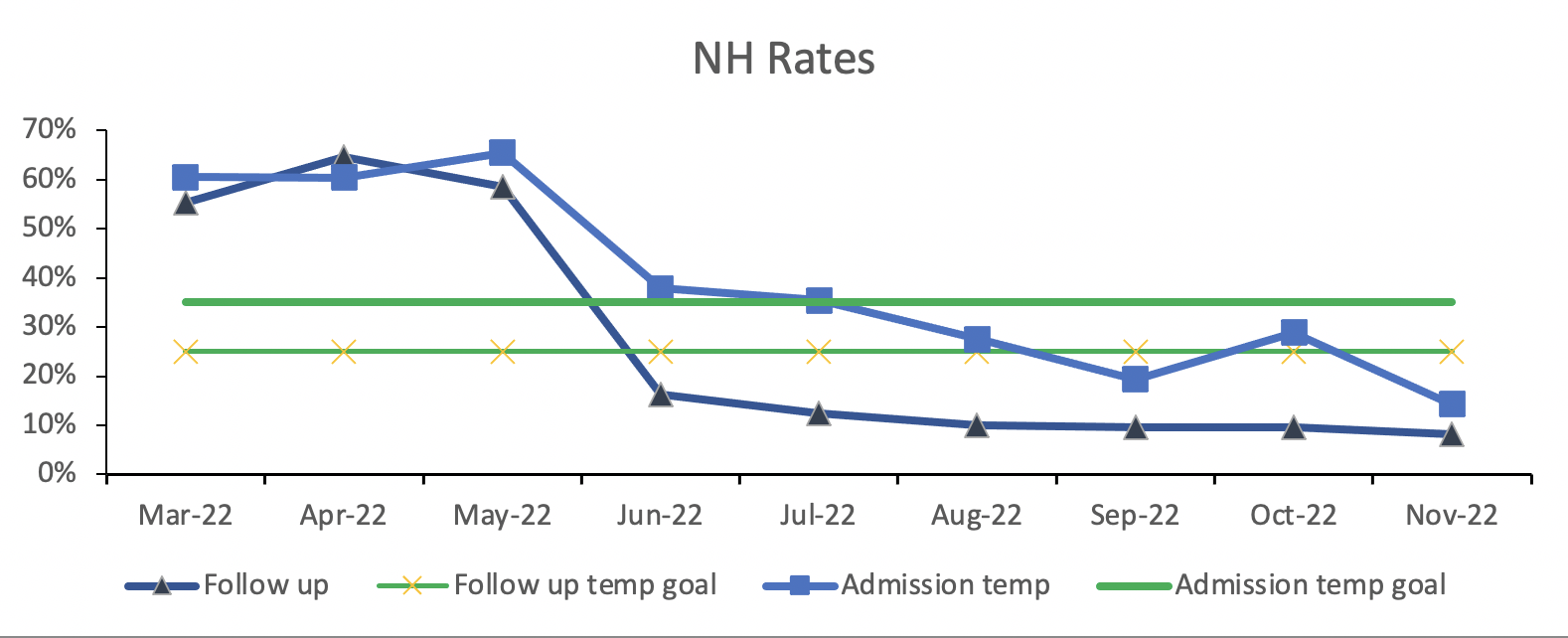
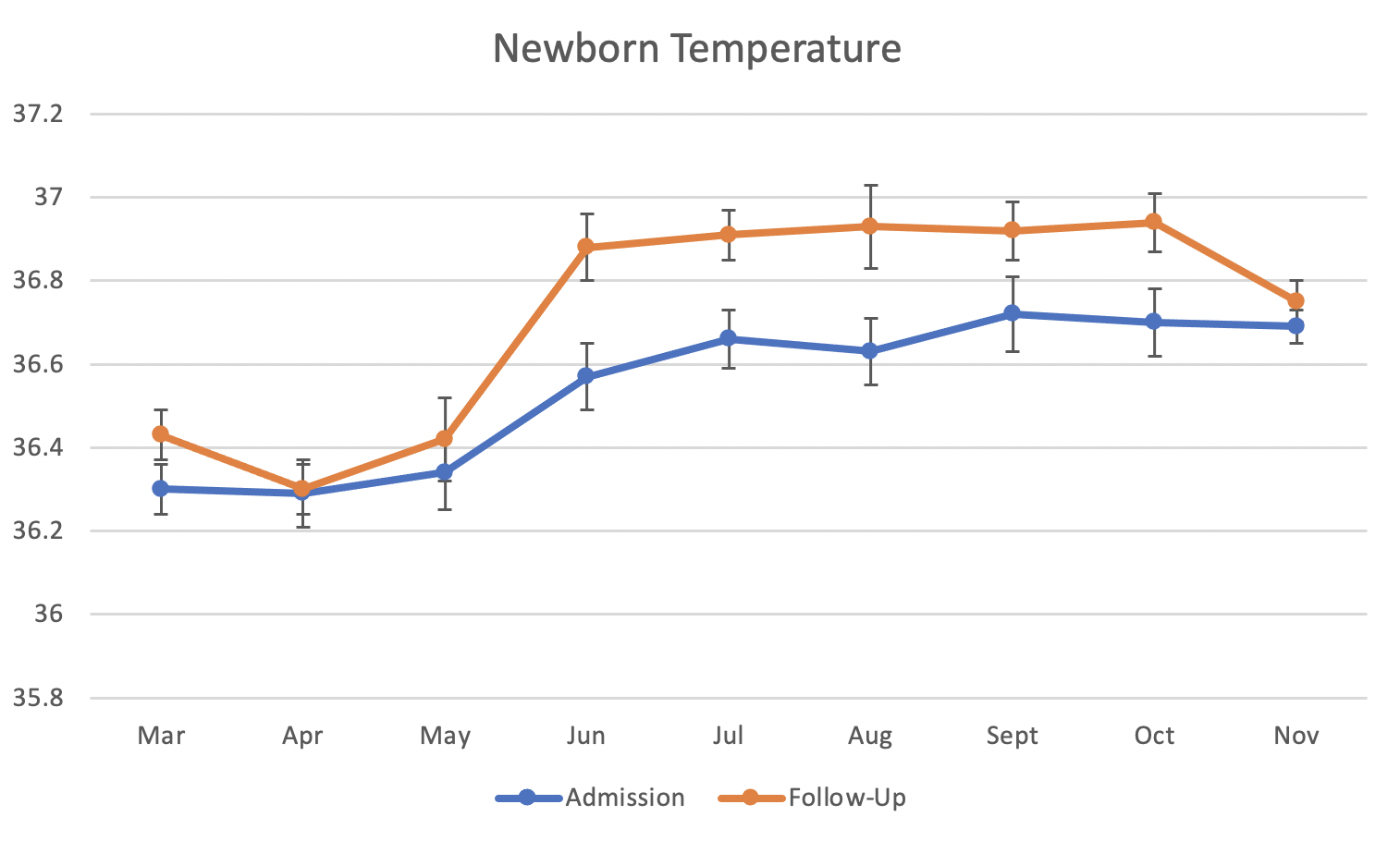
Design/Methods: The study consisted of a three month baseline Pre-Intervention phase, the intervention (education and the introduction of the Infant Warmers), and a six month Warmer Use phase. We included all newborns admitted to the neonatal ward. During both the Pre-Intervention and Warmer Use phases, we collected temperature data on admission to the neonatal ward and 6 hours later, called “follow up” temperatures. We collected qualitative survey data from healthcare workers regarding their knowledge of neonatal hypothermia and their confidence in keeping babies warm.
Results:
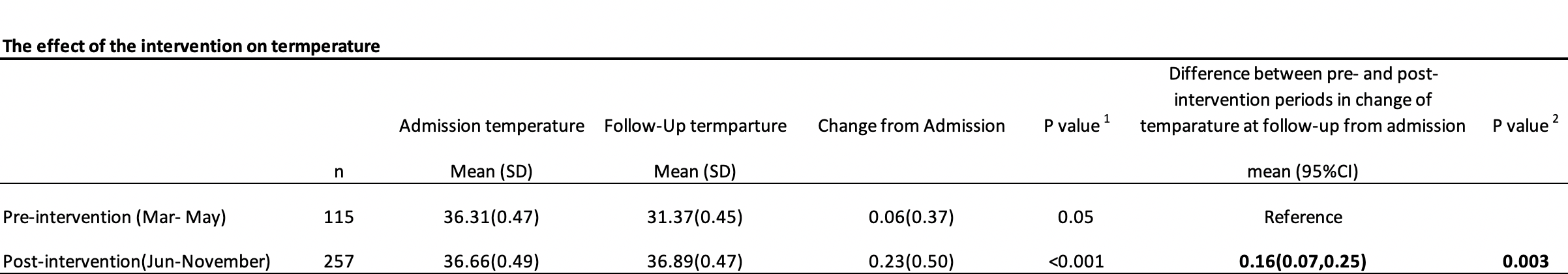
We studied a total of 372 newborns, 115 Pre Intervention and 257 during the Warmer Use phase. Baseline rates of NH on admission were 62%, falling to 27% in the Warmer Use phase. Baseline rates of NH on follow-up were 59%, falling to 11% during Warmer Use. The mean admission temperature rose from 36.31 C baseline to 36.66 C during Warmer Use (p= 0.05). The follow up temperature rose from 36.37C baseline to 36.89C during Warmer Use (p=< 0.001). Thus, the ability to warm newborns in the 6 hours following the diagnosis of hypothermia on admission temperature improved significantly from 0.06C pre intervention to 0.23C during Warmer Use (p=0.003). Healthcare workers' ability to correctly define hypothermia was 38% at baseline, rising to 86% by the end of the study. Similarly, 30% reported being confident in keeping newborns warm at baseline, rising to 87% by the end of the study.
Conclusion(s):
We found unacceptably high rates of NH in this low resourced hospital. We successfully lowered rates and improved knowledge of NH employing an implementation science approach with education and the provision of appropriate thermoregulatory equipment to preserve the heat chain.