Neonatal Quality Improvement
Neonatal Quality Improvement 3
727 - A Late Preterm Quality Improvement Bundle to Decrease Morbidity and Prevent NICU Admission
Publication Number: 727.342

Amy L. Lembeck, DO (she/her/hers)
Neonatologist
Childrens Hospital of Philadelphia
Newtown Square, Pennsylvania, United States
Presenting Author(s)
Background: Late preterm infants (35 0/7 to 36 6/7 weeks, LPI) are at greater risk for morbidity including NICU admission and prolonged length of stay. This cohort of infants is often grouped with term healthy infants and their risk factors often go unaddressed. Due to their prematurity, this population is at risk for hypothermia, hypoglycemia, and respiratory distress. These morbidities often result in NICU admission.
Objective: We sought to decrease NICU admission of late preterm infants by 10% within 12 months.
Design/Methods: Baseline data were collected at our 1900 delivery level 3 NICU community hospital in Pennsylvania which excluded infants < 35 weeks and < 2 kg as they were automatically admitted to the NICU. Multidisciplinary discussion occurred across the Delivery Unit to focus on areas of improvement. With evaluation of feeding to maintain euglycemia, interventions to improve euthermia, and a tailored LPI order-set, the team monitored data with control charts. Multiple education sessions helped to reinforce change and behaviors. Additional data monitored reason for admission to NICU, breast feeding success, and length of stay.
Results:
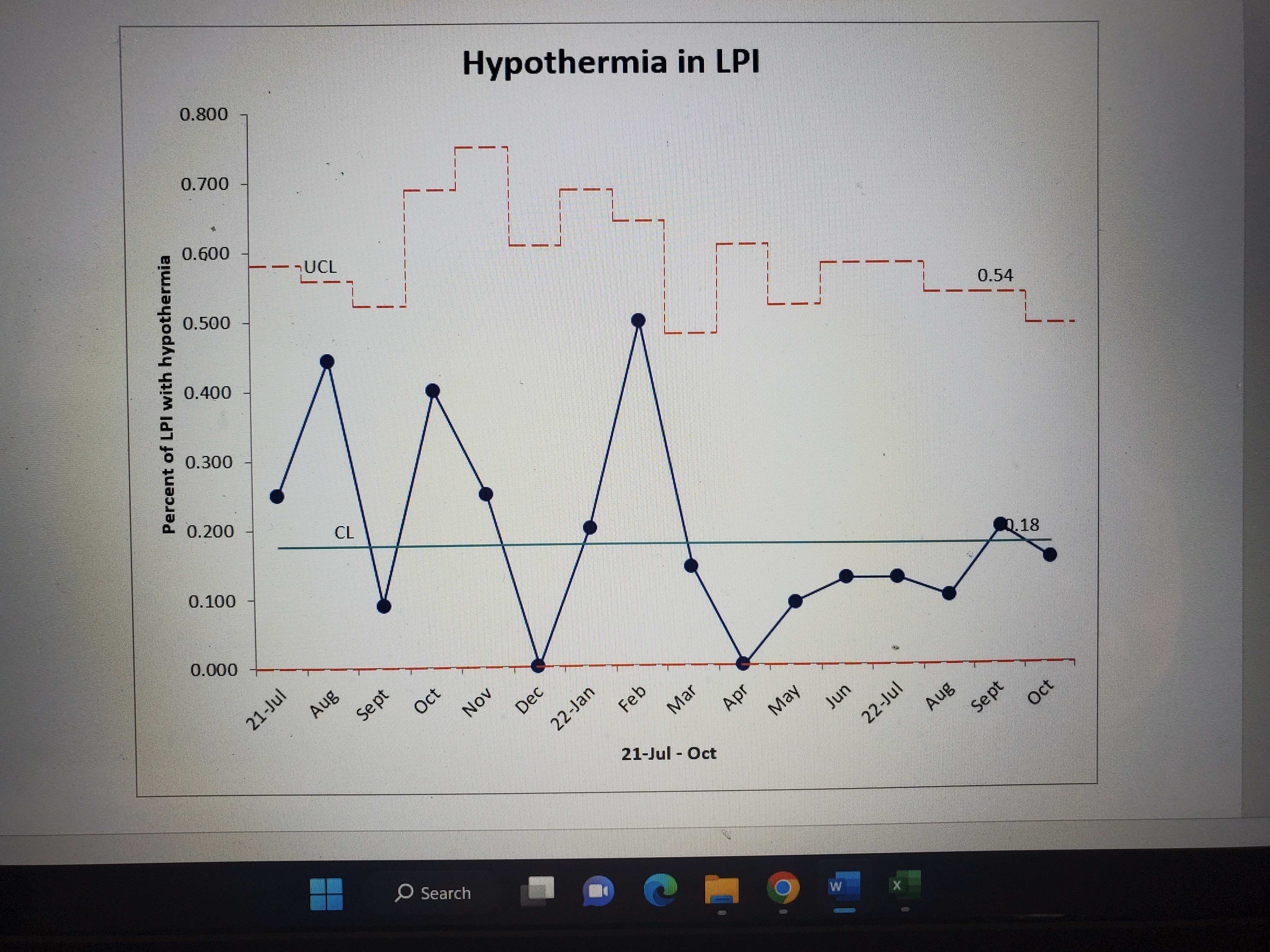
Of all infants admitted to the Post-Partum Unit (PPU), 159 LPIs over a 2 year period had data. NICU admission rates did not decrease consistently over the 2 year period. 32.6% of LPI admitted to PPU required NICU admission at initiation of our interventions. 30% of infants at time of analysis required NICU admission. There were time spans with a lower rate of NICU admission but they were not maintained for greater than 5 months. 59% of NICU admissions were for respiratory distress, a potentially non-modifiable morbidity. 8% were for hypothermia, 8% for hypoglycemia and 25% for other causes. Hypoglycemia in LPI infants remained constant despite modifications in calories and the adoption of glucose gel. Hypothermia is trending towards statistical change. Process measures included LPI order-set use and a LPI educational pamphlet. Both were adopted as process measures after successful implementation as an intervention.
Conclusion(s): Through an improvement bundle utilizing education, formalized orders, and modifications to improve euthermia and euglycemia, our team has been unable to modify the number of LPI admitted to the NICU. Our data is trending towards improvement with less variability but has not indicated sustainable change at this time. A closer look at why the LPI is admitted may help to focus on additional modifiable morbidities. Reporting and sharing this information is helpful for other units seeking to improving their outcomes in the LPI population.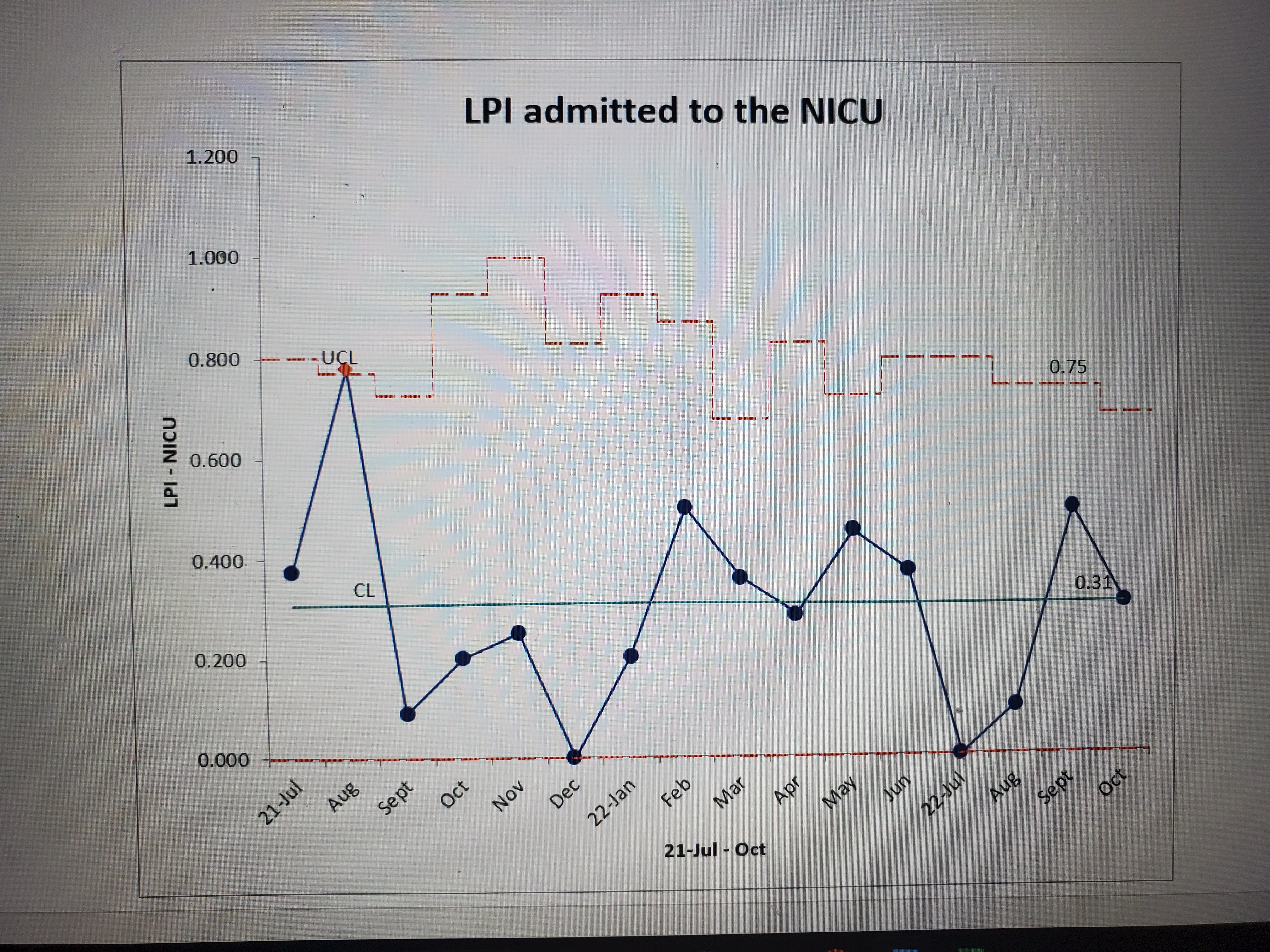
.jpg)